Relationship between Metabolic Syndrome and Uterine Leiomyoma: A Case Control Study
DOI:
https://doi.org/10.60787/tnhj.v24i1.765Keywords:
Leiomyoma, Metabolic syndrome (Mets), Obesity, BMI (Body mass index), Case control studyAbstract
Background: Uterine leiomyoma is the most common benign gynaecological tumour of the female reproductive tract. Although, the cause of uterine leiomyoma is still unclear; however, studies have shown that single and multiple components of metabolic syndrome such as hypertension, obesity, elevated triglycerides, and type 2 diabetes may be associated with the prevalence of uterine leiomyoma.
Method: This is a prospective case-control study conducted in the Department of Obstetrics and Gynaecological of the Lagos State University Teaching Hospital from 26th March 2020 to September 28th, 2020. This study aimed to evaluate the associations between metabolic syndrome and uterine leiomyoma. A total of 165 cases were recruited and analysed for both the study population and control. All data was imputed onto a proforma. Statistical analysis was done using the Statistical Package for Social Science (SPSS) version 22. Conditional logistic regression was used to examine the associations between independent variables and uterine leiomyoma.
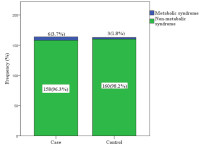
Result: There was no statistically significant difference in the prevalence of metabolic syndrome between participants in the fibroid and non-fibroid group (3.7% vs1.8%, P=0.315). Prevalence of obesity and hyperglycaemia were significantly higher in the leiomyoma group compared to the control group (77.4% vs 20.2%, P<0.001 and 6.7% vs 1.8%, P=0.028. Regression analysis showed a three-fold risk of uterine fibroids among cases when waist circumference was elevated, (OR=3.876;95% CI,1.759-7.981).
Conclusion: There was no significant association between the prevalence of metabolic syndrome and uterine leiomyomas, however, the prevalence of obesity and hyperglycaemia were significantly associated with uterine leiomyoma.
Downloads
References
Parker W. Uterine Myoma management. Fertil Steril. 2007;88(2):255–71.
Ogunniyi S, Fasubaa O. Uterine Fibromyoma in Ilesha, Nigeria. Niger Med Pract. 1990;19(6):93–5.
Emembolu J. Uterine Fibromyomata : presentation and management in Northern Nigerian. Int J Gynaecol Obstet. 1987;25(5):413–6.
Aboyeji A, Ijaiya M. Uterine Fibroids: a ten-year clinical review in Ilorin, Nigeria. Niger J Med. 2002;11(1):16–9.
Anate M. Uterine fibroids in Federal Medical Centre, Lokoja: A five year review 2002-2006. Niger Clin Rev J. 2007; 1:5–12.
Okezie O, Ezeugwu H. Management of Uterine fibroids in Enugu. Niger J Obstet Gyneacology. 2006;26(4):363–5.
Wilcox L, Koonin L. Hysterectomy in the United States. Obstet Gynaecol. 2006;26(4):363–5.
Walker C, Stewart E. Uterine fibroids: the elephant in the room. Science. 2005;308(5728):1589–92.
Sparic R, Mirkovic L, Malvasi A. Epidemiology of uterine myomas: A Review. Int J fertilty Steril. 2016;9(4):424–35.
Marshall L, Spiegelman D, Barbieri R. Variation in the incidence of uterine leiomyoma among premenopausal women by age and race. Obstet Gynaecol. 1997;90(6):967–73.
Faerstein E, Szklo M, Rosenshein N. Risk factors for uterine leiomyoma: a practice-based case-control study. I. African-American heritage, reproductive history, body size and smoking. Am J Epdemiology. 2001;153(1):1–10.
Gross K, Morton C. Genetics and the development of fibroids. Clin Obstet Gynaecol. 2001;44(2):335–49.
Sato F, Mori M, Nishi M. Familial aggregation of uterine myoma in Japanese women. J Epidemiol. 2002;12(3):249–53.
Luoto R, RUtanen E, Auvinen A. Fibroids and hypertension: a cross-sectional study of women undergoing hysterectomy. J Reprod Med. 2001;46(4):359–64.
Okoronkwo M. Body weight and uterine leiomyomas among women in Nigeria. West Afr J Med. 1999;18(1):52–4.
Chiaffarino F, Parazzini F, La Vecchia C. Diet and uterine myomas. Obstet Gynaecol. 1999;94(3):395–8.
Deedwania P, Gupta R. Management issues in Metabolic Syndrome. J Assoc Physician, India. 2006;54(1):797–810.
Reaven G. Metabolic Syndrome: pathophysiology and implication for management of cardiovascular disease. Circulation. 2002;106(3):286–8.
Charan J, Biswas T. How to calculate sample size for different study designs in medical research. Indian J Psychol Med. 2013;35(2):121–6.
Alberti K, Eckel R, Grundy S. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung and Blood Institute; America Heart Association; World Heart Federation; International At. Circulation. 2009;120(16):1640–5.
Tak J, Lee Y, Park S. Association between uterine leiomyoma and metabolic syndrome in parous premenopausal women. A case-control study. Medicine (Baltimore). 2012;95(46):e5325.
Moon K, Ryu S, Kim K. Relationship between Metabolic syndrome and Uterine Fibroids in premenopausal Korean women: A case-control study. Korean J Fam Pr. 2013;3(3):437–41.
Takeda T, Sakata M, Isobe A. Relationship between Metabolic syndrome and Uterine leiomyomas: A case-control study. Gynecol Obs Invest. 2008;66(1):14–7.
BeLue R, Okoror T, Iwelunmor J. An overview of cardiovascular risk factor burden in sub-Saharan African countries: A socio-cultural perspective. Glob Heal. 2009;5(3):10.
Uimari O, Auvinen J, Jokelainen J. Uterine fibroids and cardiovascular risk. Hum Reprod. 2016;31(12):2689–703.
Babah OA, Oluwole AA, Afolabi BB. Effect of obesity on the development of uterine leiomyoma: a rerospective study of 169 women who had myomectomy in southern Nigeria. JOSR-JDMS 2014;13(3):74-78.
Antai D, Moradi T. Urban area disadvantage and under 5 mortalities in Nigeria: The effect of rapid urbanization. Env Heal Perspect. 2010;118(6):877–88.
Baird D, Travois G, Wilson R. Uterine leiomyomata in relation to insulin-like growth factor-1, Insulin and diabetes. Epidemiology. 2009;20(4):604–10.
Faerstein E, Szklo M, Rosenshein N. Risk factors for uterine leiomyoma: a practice-based case-control study. II. Atherogenic risk factors and potential sources of uterine irritation. Am J Epdemiology2. 2001;153(1):11–9.
Hou ZM, Sun Q, Liu YZ, Chen TF, Tang N. Effects of insulin resistance on myometrial growth. Int J Clin Exp Med. 2015 Jan 15;8(1):1552-7.
Wise LA, Laughlin-Tommaso SK. Epidemiology of Uterine Fibroids: From Menarche to Menopause. Clin Obstet Gynecol. 2016 Mar;59(1):2-24.
Parazzini F. Risk factors for clinically diagnosed uterine fibroids in women around menopause. Maturitas. 2006;55(2):174–9.
Daniel O, Adejumo O, Adejumo E. Prevalence of hypertension among urban slum dwellers in Lagos, Nigeria. J Urban Heal. 2013; 90:1016–25.
Jarrett R, Edward R, Malspeis S. A prospective study of hypertension and risk of uterine leiomyomata. Am J Epidemol. 2005;161(1):628–38.
He Y, Zeng Q, Li X. The association between subclinical artherosclerosis and uterine fibroids. PLoS One. 2013;8(2):e57089.
Published
Issue
Section
License
Copyright (c) 2024 Journal and Publisher

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
The Journal is owned, published and copyrighted by the Nigerian Medical Association, River state Branch. The copyright of papers published are vested in the journal and the publisher. In line with our open access policy and the Creative Commons Attribution License policy authors are allowed to share their work with an acknowledgement of the work's authorship and initial publication in this journal.
This is an open access journal which means that all content is freely available without charge to the user or his/her institution. Users are allowed to read, download, copy, distribute, print, search, or link to the full texts of the articles in this journal without asking prior permission from the publisher or the author.
The use of general descriptive names, trade names, trademarks, and so forth in this publication, even if not specifically identified, does not imply that these names are not protected by the relevant laws and regulations. While the advice and information in this journal are believed to be true and accurate on the date of its going to press, neither the authors, the editors, nor the publisher can accept any legal responsibility for any errors or omissions that may be made. The publisher makes no warranty, express or implied, with respect to the material contained herein.
TNHJ also supports open access archiving of articles published in the journal after three months of publication. Authors are permitted and encouraged to post their work online (e.g, in institutional repositories or on their website) within the stated period, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See The Effect of Open Access). All requests for permission for open access archiving outside this period should be sent to the editor via email to editor@tnhjph.com.





