Comparative Assessment of Childhood Overweight and Obesity among Public and Private Schools Pupils in Obio/Akpor Local Government Area, Rivers State, Nigeria
Main Article Content
Abstract
Background: Childhood overweight and obesity is a risk factor for the onset of chronic non-communicable diseases like type II diabetes and hypertension. Between May and August 2019, researchers conducted this study in Obio/Akpor to compare the prevalence of overweight and obesity among pupils attending public and private elementary schools.
Method: The research was a comparative descriptive study. In Obio/Akpor Local Government Area of Port Harcourt, Nigeria, 1040 pupils aged 6-12 years from public and private elementary schools were assessed. The pupils' height and weight were measured in order to determine their body mass index. Chi-square test was used for test statistics. To gather pertinent information, a semi-structured questionnaire was utilized. The significance criterion for each statistical test was set at P 0.05.
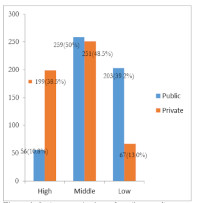
Result: A total of 205 (19%) pupils in public and private schools out of the 1035 pupils who later completed study were found to be overweight or obese. Pupils in private schools made up the majority of cases, with 82 (15.9%) and 49 (9.5%) of them being overweight and obese, respectively, as opposed to 41 (7.9%) and 33 (6.4%) of pupils in public schools. The difference in overweight and obesity among the private and public school was statistically significant (, P=0.001). Higher socioeconomic class was significantly associated with the higher prevalence (P<0.001).
Conclusion: The prevalence of childhood overweight and obesity was high in both study populations, while it was significantly higher among students enrolled in private primary schools.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Journal is owned, published and copyrighted by the Nigerian Medical Association, River state Branch. The copyright of papers published are vested in the journal and the publisher. In line with our open access policy and the Creative Commons Attribution License policy authors are allowed to share their work with an acknowledgement of the work's authorship and initial publication in this journal.
This is an open access journal which means that all content is freely available without charge to the user or his/her institution. Users are allowed to read, download, copy, distribute, print, search, or link to the full texts of the articles in this journal without asking prior permission from the publisher or the author.
The use of general descriptive names, trade names, trademarks, and so forth in this publication, even if not specifically identified, does not imply that these names are not protected by the relevant laws and regulations. While the advice and information in this journal are believed to be true and accurate on the date of its going to press, neither the authors, the editors, nor the publisher can accept any legal responsibility for any errors or omissions that may be made. The publisher makes no warranty, express or implied, with respect to the material contained herein.
TNHJ also supports open access archiving of articles published in the journal after three months of publication. Authors are permitted and encouraged to post their work online (e.g, in institutional repositories or on their website) within the stated period, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See The Effect of Open Access). All requests for permission for open access archiving outside this period should be sent to the editor via email to editor@tnhjph.com.
How to Cite
References
WHO. Global Strategy on Diet, Physical Activity & Health. In: report of a WHO forum and technical meeting, Geneva. 2016. Retrieved from https://www.who.int/dietphysicalactivity/childhood/en/
Musa DI, Toriola AL, Monyeki, MA. Prevalence of Childhood and Adolescent Overweight and Obesity in Benue State, Nigeria. Tropical Medicine & International Health: TM & IH. 2012; 17:1369-1375.https://doi.org/10.1111/j.1365-3156.2012.03083.x
WHO. Obesity and overweight. 2018. Retrieved from http://www.who.int/mediacentre/factsheets/fs311/en
Ofakunrin et al. Prevalence of overweight and obesity among school-age children in Jos, North Central, Nigeria. Intr Journ of Biomedl Research. 2018;9(06), 208-213. https://doi.org/DOI: https://doi.org/10.7439/ijbr
Carter M. Parents and School Choice: What are the implications? 2018. Retrieved from https://www.edcan.ca/articles/parents-school-choice-implications/
Guillermo M, Wippold G,Tucker C. Childhood obesity disparities: Influential factors and intervention strategies Socioeconomic, cultural, family, community/environmental and psychological factors contribute to racial/ethnic disparities of childhood obesity. CYF News. 2016. Retrieved from https://www.apa.org/pi/families/resources/newsletter/2016/06/childhood-obesity
Eke C, Ubesie A, Ibe B. Challenges of childhood obesity in a developing economy: A review. Nigr J of Pedtr 2015;42(3), 169-179–179.
WHO. Report of the commission on ending childhood obesity. 2016; https://doi.org/ISBN 978 92 4 151006 6
Small L, Aplascare A. Child Obesity and Mental Health: A Complex Interaction. 2018; https://doi.org/https://doi.org/10.1016/j.chc.2015.11.008
Larson K, Slusser W, Halfon N, Associations between obesity and comorbid mental health, developmental, and physical health conditions in a nationally representative sample of US children aged 10 to 17. Acad Pediatr. 2013; 13:6–13. [PubMed] [Google Scholar]
Tochie J, Mbonda A, Fonkwo V, Aletum, V. Childhood Overweight and Obesity in Sub-Saharan Africa : Current Definition, Prevalence and Risk Factors. acta sci pedtric 2018;2(8), 37-40. https://doi.org/DOI: 10.31080/ASPE.2019.02.0110
WHO. Stronger focus on nutrition within health services could save 3.7 million lives by 2025. Retrieved from https://www.who.int/news-room/detail/04-09-2019-stronger-focus-on-nutrition-within-health-services-could-save-3.7-million-lives-by-2025. 2019.
Khadilkar V, Khadilkar A, Cole, T et al. Overweight and obesity prevalence and body mass index trends in Indian children. Int J Pediatr Obes. 2011;6(2), 216-24. https://doi.org/doi: 10.3109/17477166.2010.541463.
Klingberg S, Draper C, Micklesfield L, et al. Childhood Obesity Prevention in Africa: A Systematic Review of Intervention Effectiveness and Implementation. Int J Environ Res Public Health.2019; 16(7). https://doi.org/doi: 10.3390/ijerph16071212
WHA. Seventy-First World Health Assembly. digital health. Retrieved from https://www.google.com/search?q=ehealth+strategies&oq=eHealth+strategies&aqs=chrome.0.0l4.3159j0j8&sourceid=chrome&ie=UTF-8. 2018.
WHO. International statistical classification of disease and health related condition. ICD-11 for Mortality and Morbidity Statistics. 2019.
Ogbo P, Aina B, Obettah, N. Increasing burden of obesity among children 5-11 years old in Lagos Nigeria. Retrieved from Obesity Reviews website: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed12&NEWS=N&AN=71516390. 2014
Sadoh W, Sadoh A, Onyiriuka, A. Physical activity, body mass index and blood pressure in primary school pupils attending private schools. Afr Health Sci..2016;16(4), 947-953. https://doi.org/doi: 10.4314/ahs. v16i4.10.
Aigbogun EJ, Ibeachu P, Ikechukwu E. BMI-For-Age Cut-Off as an Indicator of Adiposity among In-School Children (Age 4-11 Years) in Obio/Akpor LGA, Rivers State, Nigeria. Int J of Pedtric Health Care & Advanc (IJPA), 2017;4(7), 63-69. Retrieved from ISSN 2572-7354
Ade F, Odukoya O, Oyeyemi A et al. Results From Nigeria’s 2016 Report Card on Physical Activity for Children and Youth. Journal of Physical Activity and Health,.2016; 13 S(2), 231-S236. https://doi.org/http://dx.doi.org/10.1123/jpah.2016-0305
Obio/Akpor Local Government Educational Authority (OBALGEA) https://www.manpower.com.ng/company/238718/obio-akpor-local-government-education-authority-office. 2019.
Brinkhoff T. Obio/Akpor Local Government Area in Nigeria. In city population-statistics,maps and charts.2017
Kelsey MM, Zaepfel A, Bjornstad P, Nadeau K. Age-related consequences of childhood obesity. Gerontology. Epub 2014;60(3):222-8. doi: 10.1159/000356023. PMID: 24434909.
Sadoh W, Sadoh A, Onyiriuka A Physical activity, body mass index and blood pressure in primary school pupils attending private schools. Afr Health Sci. 2017.16(4), 947-953. https://doi.org/doi: 10.4314/ahs. v16i4.10.
CDC. Centers for Disease Control and Prevention/National Center for Health Statistics. 2000 CDC Growth Chart for the United States: Methods and Development. Vital and Health Statistics. 2002; 11(246).
Ogunlesi AT, Dedeke IF, Kuponiyi,O.T (2008)Socio-economic classification of children attending specialist paediatric centres in Ogun State, Nigeria. Vol. 54 No. 1 (2008) DOI:10.4314/nmp.v54i1.28943 https://www.ajol.info/index.php/nmp/article/view/28943
Ajayi E, Elechi IH, Alhaji1 M. No Title. Saudi J of Obes. 2015; 3(2). https://doi.org/DOI: 10.4103/2347-2618.171959
Mezie-Okoye M, Alex-Hart B. No Title. Pakistan J of Nutr 2015; 14(4), 209–213.
Salman Z, Kirk G, DeBoer M. High Rate of Obesity-Associated Hypertension among Primary Schoolchildren in Sudan. Int J of Htn،, 2011; 1–5.
Bello S et al. Overweight and Obesity among School Children Aged 6- 12 Years in Illorin North Central Nigeria. IOSR-JDMS 2018; 17(7), 37–41. https://doi.org/DOI: 10.9790/0853-1707013741