Tuberculosis Treatment Outcomes and Determinants of Treatment Default in a Tertiary Health Facility in Obio/Akpor Local Government Area, Rivers State
Main Article Content
Abstract
Background: The study aimed to assess tuberculosis treatment outcomes, and the factors associated with treatment default among patients who received TB treatment at the Directly Observed Treatment Short Course (DOTS) clinic of the University of Port Harcourt Teaching Hospital
Materials and Methods: A cross-sectional study design was used to retrospectively review tuberculosis cases at the DOTS Clinic from January 1, 2019, to December 17, 2023. The research examined 342 files/records. Data was analysed using SPSS version 27. Pearson's Chi-square test was used to determine the association between the outcome and independent variables at P ≤ 0.05 statistical significance level.
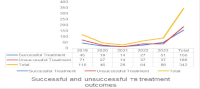
Result: The result shows that mean age of 31.5±17.9, 89 (26.0%) of the cases seen were less than 20 years old, 187 (54.7%) were males, and 213 (62.3%) were singles. Fifty-three (15.5%) were cured, 103 (30.1%) of the respondents completed treatment, 81(23.7%) defaulted, 69 (20.2%) lost to follow-up, 3 (0.9%) were treatment failures and 14 (4.15%) died. The overall treatment success rate was 156 (45.6%), 35 (38.8%) in 2019 and 51 (57.9%) in 2023. Sputum positivity (χ2 = 31.34; p < 0.001) and HIV status (χ2 = 11.75; p < 0.007) were significantly associated with treatment success rate, only sputum positivity (χ2 = 7.726; p < 0.038) was associated with default P≤0.05.
Conclusion: The treatment success rate was lower than the World Health Organisation’s cut-off mark (85.0%). The default rate was also high. Strategies should be developed to enhance optimum TB treatment outcomes in Rivers State, Nigeria.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
The Journal is owned, published and copyrighted by the Nigerian Medical Association, River state Branch. The copyright of papers published are vested in the journal and the publisher. In line with our open access policy and the Creative Commons Attribution License policy authors are allowed to share their work with an acknowledgement of the work's authorship and initial publication in this journal.
This is an open access journal which means that all content is freely available without charge to the user or his/her institution. Users are allowed to read, download, copy, distribute, print, search, or link to the full texts of the articles in this journal without asking prior permission from the publisher or the author.
The use of general descriptive names, trade names, trademarks, and so forth in this publication, even if not specifically identified, does not imply that these names are not protected by the relevant laws and regulations. While the advice and information in this journal are believed to be true and accurate on the date of its going to press, neither the authors, the editors, nor the publisher can accept any legal responsibility for any errors or omissions that may be made. The publisher makes no warranty, express or implied, with respect to the material contained herein.
TNHJ also supports open access archiving of articles published in the journal after three months of publication. Authors are permitted and encouraged to post their work online (e.g, in institutional repositories or on their website) within the stated period, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See The Effect of Open Access). All requests for permission for open access archiving outside this period should be sent to the editor via email to editor@tnhjph.com.
How to Cite
References
1. World Health Organization. Global Tuberculosis Report 2024 [Internet]. [cited 2025 Mar 3]. Available from: https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2024
2. World Health Organization. Global Tuberculosis Control. 2011.
3. WHO. Global Tuberculosis Report 2018. Geneva: 2018.
4. WHO. Tuberculosis [Internet]. [cited 2022 Jan 21]. Available from: https://www.who.int/news-room/fact-sheets/detail/tuberculosis
5. Bagcchi S. WHO’s global tuberculosis report 2022. The Lancet Microbe. 2023 Nov 22;4(1):e20.
6. George DM, Bibiye AAS. Compliance to Tuberculosis Treatment Across Medical Institutions in Rivers State, South-South Nigeria. International Journal of Health and Psychology Research. 2022 Nov 22; 8:9.
7. FMOH. Department of Public Health & Leprosy Control Programme Nigeria 2014 NTBLCP Annual Report. 2014.
8. Chakaya J, Khan M, Ntoumi F, Aklillu E, Fatima R, Mwaba P, et al. Global Tuberculosis Report 2020 – Reflections on the Global TB burden, treatment and prevention efforts. International Journal of Infectious Diseases. 2021 Nov 23;113(S): S7–12.
9. Izudi J, Tamwesigire IK, Bajunirwe F. Treatment success and mortality among adults with tuberculosis in rural eastern Uganda: a retrospective cohort study. BMC Public Health. 2020 Nov 23;20(1):501.
10. Shilongo E. Treatment Outcomes and Associated Factors in TB/HIV-Coinfected Patients in Namibia. Walden University; 2022.
11. Izudi J, Semakula D, Sennono R, Tamwesigire IK, Bajunirwe F. Treatment success rate among adult pulmonary tuberculosis patients in sub-Saharan Africa: a systematic review and meta-analysis. BMJ Open. 2019 Sep;9(9):e029400.
12. Des-Wosu I, Owhonda G, Tobin-West CI. Spatial-temporal Distribution of Tuberculosis Infections in Rivers State from 2009-2018. Journal of Epidemiological Society of Nigeria. 2021 Nov 23;4(2):7–12.
13. Ogbonna V, Alabere D, Tobin-West C. Treatment outcomes and associated factors of tuberculosis patients on directly observed treatment (short course) in a tertiary hospital in Port Harcourt, Nigeria. Nigerian Journal of Medicine. 2020;29(4):707–13.
14. National Tuberculosis and Leprosy Control Programme. 2019 Annual TB report. 2019.
15. Israel GD. Determining sample size. 1-5. 2009.
16. Alao MA, Maroushek SR, Chan YH, Asinobi AO, Slusher TM, Gbadero DA. Treatment outcomes of Nigerian patients with tuberculosis: A retrospective 25-year review in a regional medical center. Wingfield TE, editor. PLOS ONE. 2020 Nov 23;15(10):e0239225.
17. Tesfahuneygn G, Medhin G, Legesse M. Adherence to Anti ‑ tuberculosis treatment and treatment outcomes among tuberculosis patients in Alamata District, Northeast Ethiopia. BMC Research Notes. 2015;11(691):1–11.
18. Inotu A, Abebe F. Assessment of defaulting from directly observed treatment short course (DOTS) and its determinants in Benin City, Nigeria. Journal of Tuberculosis Research. 2014 Nov 25;2014.
19. Daniels OJ, Oladapo OT, Alausa OK. Default from tuberculosis treatment programme in Sagamu, Nigeria. Nigerian Journal of Medicine. 2006 Nov 25;15(1):63–7.
20. Azuogu B, Eze N, Azuogu V, Emegoakor A, Osuagwu A, Inya A, et al. Prevalence and Predictors of Tuberculosis Treatment Default in Abakaliki, Nigeria: An Implication for Patient Centred Education and Treatment Follow-Up. International Journal of TROPICAL DISEASE & Health. 2018 Nov 25;29(1):1–9.
21. Chan-Yeung MMW, Noertjojo K, Leung CC, Chan SL, Tam CM. Prevalence and predictors of default from tuberculosis treatment in Hong Kong. 2003 Nov 25.
22. Umeokonkwo CD, Okedo-Alex IN, Azuogu BN, Utulu R, Adeke AS, Disu YO. Trend and determinants of tuberculosis treatment outcome in a tertiary hospital in Southeast Nigeria. Journal of Infection and Public Health. 2020 Nov 25;13(7):1029–33.