Staff-related Predictors of Knowledge and Practice of Clinical Audit among Doctors in a Tertiary Health Facility in a Developing Country: A Cross-Sectional Study
DOI:
https://doi.org/10.60787/tnhj.v24i4.939Keywords:
Predictors, knowledge, practice, clinical audit, doctors, University of Port Harcourt Teaching HospitalAbstract
Background: Clinical auditing lowers mortality and morbidity and enhances the quality of patient care. This study identified staff-related determinants of the knowledge and practice of clinical audit (CA) among physicians in a Nigerian tertiary facility.
Method: Convenience sampling of 460 doctors was employed in this descriptive cross-sectional study using pre-tested questionnaires. Frequency distributions, binary and multivariate logistic regression were conducted using SPSS 23.0. A P-value ≤0.05 was considered significant for the inferential statistics.
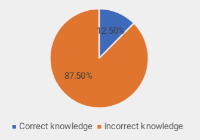
Results: A response rate of 99.3% was obtained from the analysis of 457 questionnaires. Out of these, only 57 (12.5%) clearly understood the CA process. Those who are consultants (AOR 44.2, 95%CI:4.6, 425.5; p = 0.001), senior registrars (AOR 14.8, 95%CI:1.7, 126.0; p = 0.014), and registrars (AOR 10.2, 95%CI:1.3, 79.0; p = 0.027) were significantly more knowledgeable in CA compared to Interns. Mortality reviews were commoner in Surgery (p=0.021), Obstetrics/gynaecology (p=0.027) and Paediatrics (p<0.001) than in other specialties. Consultants were more involved in mortality audits (p=0.05) compared to other cadres. Survey of patient experiences, process audits and cost of care analyses were more common among physicians with 10-19 years in practice.
Conclusion: Significant gaps exist the knowledge and practice of CA among doctors in this tertiary hospital. Addressing these deficiencies requires targeted efforts in education, policy interventions, and institutional reforms to strengthen clinical governance and improve quality of care.
Downloads
References
Weiner S, Schwartz A, Altman L, Ball S, Bartle B, Binns-Calvey A, Chan C, Falck-Ytter C, Frenchman M, Gee B, Jackson JL. Evaluation of a patient-collected audio audit and feedback quality improvement program on clinician attention to patient life context and health care costs in the veterans affairs health care system. JAMA network open. 2020 Jul 1;3(7): :e209644-
Willis TA, Wood S, Brehaut J, Colquhoun H, Brown B, Lorencatto F, Foy R. Opportunities to improve the impact of two national clinical audit programmes: a theory-guided analysis. Implementation Science Communications. 2022 Mar 21;3(1):32.
Sarkies M, Francis-Auton E, Long J, Roberts N, Westbrook J, Levesque JF, Watson DE, Hardwick R, Sutherland K, Disher G, Hibbert P. Audit and feedback to reduce unwarranted clinical variation at scale: a realist study of implementation strategy mechanisms. Implementation Science. 2023 Dec 11;18(1):71.
Van Der Winden, D., Van Dijk, N., Visser, M.R. and Bont, J., 2023. Walking the line between assessment, improvement and learning: a qualitative study on opportunities and risks of incorporating peer discussion of audit and feedback within quality improvement in general practice. BMJ open, 13(1): e066793.
Gadhiraju A. Best Practices for Clinical Quality Assurance: Ensuring Safety, Compliance, and Continuous Improvement. Journal of AI in Healthcare and Medicine. 2023 Nov 13;3(2):186-226.
Lui CW, Boyle FM, Wysocki AP, Baker P, D’Souza A, Faint S, et al. How participation in surgical mortality audit impacts surgical practice. BMC surgery. 2017 Dec; 17:1-7.
Azevedo MJ, Azevedo MJ. The state of health system (s) in Africa: challenges and opportunities. Historical perspectives on the state of health and health systems in Africa, volume II: the modern era. 2017:1-73.
Hut-Mossel L, Ahaus K, Welker G, Gans R. Understanding how and why audits work in improving the quality of hospital care: A systematic realist review. PloS one. 2021 Mar 31;16(3)
Abu-Jeyyab M, Al-Jafari M, Moawad MH, Alrosan S, Al Mse'adeen M. The Role of Clinical Audits in Advancing Quality and Safety in Healthcare Services: A Multiproject Analysis from a Jordanian Hospital. Cureus. 2024 Feb;16(2).
Ephraim-Emmanuel BC, Ogbomade R, Idumesaro BN, Ugwoke I. Knowledge, attitude and practice of preventing the occurrence of work-related musculoskeletal disorders among doctors in University of Port-Harcourt Teaching Hospital. Journal of Medical Research and Innovation. 2019 Feb 17;3(2): e000161-
Launiala A. How much can a KAP survey tell us about people's knowledge, attitudes and practices? Some observations from medical anthropology research on malaria in pregnancy in Malawi. Anthropology Matters. 2009;11(1).
Clinical Services. University of Port Harcourt Teaching Hospital. Available from https://upthng.com
Cochran WG. Sampling techniques. John Wiley & Sons, New York, NY, 1977
Perumal U, Rajivlochan M, Nundy S. The importance of clinical audit in India. Current Medicine Research and Practice. 2020 May 1;10(3):110-5.
Gupta S, Menon V. Psychiatry training for medical students: A global perspective and implications for India’s competency-based medical education curriculum. Indian Journal of Psychiatry. 2022 May 1;64(3):240-51.
Fadare JO, Enwere OO, Adeoti AO, Desalu OO, Godman B. Knowledge and attitude of physicians towards the cost of commonly prescribed medicines: a case study in three Nigerian healthcare facilities. Value in health regional issues. 2020 Sep 1; 22:68-74.
Miraj SA. Effectiveness of quality clinical active audit in improving healthcare of a multispecialty hospital in a developing country. European Review for Medical & Pharmacological Sciences. 2022 Apr 15;26(8).
Anderson J, Carton E, Da Silva AS. Impact of a structured training and support program on junior doctors’ participation in clinical audits.
Pedersen MS, Landheim A, Møller M, Lien L. Acting on audit & feedback: a qualitative instrumental case study in mental health services in Norway. BMC Health Services Research. 2018 Dec; 18:1-1.
Willcox ML, Price J, Scott S, Nicholson BD, Stuart B, Roberts NW, Allott H, Mubangizi V, Dumont A, Harnden A. Death audits and reviews for reducing maternal, perinatal and child mortality. Cochrane Database of Systematic Reviews. 2020(3).
Fitzgerald E, Mlotha-Mitole R, Ciccone EJ, Tilly AE, Montijo JM, Lang HJ, Eckerle M. A pediatric death audit in a large referral hospital in Malawi. BMC pediatrics. 2018 Dec; 18:1-7.
Foy R, Skrypak M, Alderson S, Ivers NM, McInerney B, Stoddart J, Ingham J, Keenan D. Revitalising audit and feedback to improve patient care. Bmj. 2020 Feb 27;368.
Benson T, Benson A. Routine measurement of patient experience. BMJ Open Quality. 2023 Jan 1;12(1)
Palmer KS, Brown AD, Evans JM, Marani H, Russell KK, Martin D, Ivers NM. Standardising costs or standardising care? Qualitative evaluation of the implementation and impact of a hospital funding reform in Ontario, Canada. Health research policy and systems. 2018 Dec; 16:1-5.
Mremi IR, George J, Rumisha SF, Sindato C, Kimera SI, Mboera LE. Twenty years of integrated disease surveillance and response in Sub-Saharan Africa: challenges and opportunities for effective management of infectious disease epidemics. One Health Outlook. 2021 Dec; 3:1-5.
Perry YZ, Srinidhi B, Yang Z. Gender diversity and audit quality: Evidence from the pairing of audit partners. Auditing: A Journal of Practice & Theory. 2023 Nov 1;42(4):81-104.
Atkins E, Birmpili P, Glidewell L, Li Q, Johal AS, Waton S, Boyle JR, Pherwani AD, Chetter I, Cromwell DA. Effectiveness of quality improvement collaboratives in UK surgical settings and barriers and facilitators influencing their implementation: a systematic review and evidence synthesis. BMJ open quality. 2023 Apr 1;12(2)
Martinez KA, Rothberg MB. Physician gender and its association with patient satisfaction and visit length: an observational study in telemedicine. Cureus. 2022 Sep;14(9)
Sex and Gender Sensitive Research Call to Action Group, Wainer Z, Carcel C, Hickey M, Schiebinger L, Schmiede A, McKenzie B, Jenkins C, Webster J, Woodward M, Hehir A. Sex and gender in health research: updating policy to reflect evidence. Medical Journal of Australia. 2020 Feb;212(2):57-62.
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Ezioma Alinnor, Daprim Samuel Ogaji

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
The Journal is owned, published and copyrighted by the Nigerian Medical Association, River state Branch. The copyright of papers published are vested in the journal and the publisher. In line with our open access policy and the Creative Commons Attribution License policy authors are allowed to share their work with an acknowledgement of the work's authorship and initial publication in this journal.
This is an open access journal which means that all content is freely available without charge to the user or his/her institution. Users are allowed to read, download, copy, distribute, print, search, or link to the full texts of the articles in this journal without asking prior permission from the publisher or the author.
The use of general descriptive names, trade names, trademarks, and so forth in this publication, even if not specifically identified, does not imply that these names are not protected by the relevant laws and regulations. While the advice and information in this journal are believed to be true and accurate on the date of its going to press, neither the authors, the editors, nor the publisher can accept any legal responsibility for any errors or omissions that may be made. The publisher makes no warranty, express or implied, with respect to the material contained herein.
TNHJ also supports open access archiving of articles published in the journal after three months of publication. Authors are permitted and encouraged to post their work online (e.g, in institutional repositories or on their website) within the stated period, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See The Effect of Open Access). All requests for permission for open access archiving outside this period should be sent to the editor via email to editor@tnhjph.com.