Nurses’ Knowledge, Attitude, and Practice of Surgical-Patient Health Education at Modibbo Adama University Teaching Hospital, Yola
Main Article Content
Abstract
Background: Health education for surgical patients constitutes a crucial facet of patient care to alleviate associated preoperative fears and anxieties. This study evaluated nurses' knowledge, attitudes, and practices regarding Surgical-Patient Health Education (SPHE) at Modibbo Adama University Teaching Hospital in Yola, Nigeria.
Method: A descriptive cross-sectional study design was used. The sample size was electronically determined using an online application Rao-soft to achieve 140 respondents. At the same time, a proportionate purposive sampling technique was applied. A self-administered questionnaire with a reliability index of 0.72 was used to generate appropriate data and data was analyzed using IBM SPSS.
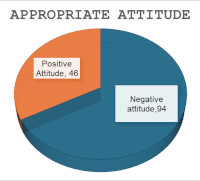
Result: The study revealed the majority of respondents were female 86(61.4%) and the mean age was 28.0±5. The findings also indicate no statistically significant relationship between the respondent’s knowledge and practice of SPHE (p=0.091). Similarly, there was no statistically significant association between selected demographic characteristics (Age, Educational qualification, and Work experience) and knowledge of SPHE (p=0.132, p=0.166, and p=0.978 respectively). However, there was a statistically significant association between work experience and practice of SPHE (p=0.020). Most of the respondents have adequate knowledge of SPHE 127(90.7%), but there was poor practice of SPHE 37(26.4%) with a corresponding negative attitude to SPHE 94(67.1%).
Conclusion: The study concludes there was adequate knowledge of SPHE among the respondents, but it did not translate to practice of SPHE. Strategies to motivate nurses to practice SPHE were recommended.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
The Journal is owned, published and copyrighted by the Nigerian Medical Association, River state Branch. The copyright of papers published are vested in the journal and the publisher. In line with our open access policy and the Creative Commons Attribution License policy authors are allowed to share their work with an acknowledgement of the work's authorship and initial publication in this journal.
This is an open access journal which means that all content is freely available without charge to the user or his/her institution. Users are allowed to read, download, copy, distribute, print, search, or link to the full texts of the articles in this journal without asking prior permission from the publisher or the author.
The use of general descriptive names, trade names, trademarks, and so forth in this publication, even if not specifically identified, does not imply that these names are not protected by the relevant laws and regulations. While the advice and information in this journal are believed to be true and accurate on the date of its going to press, neither the authors, the editors, nor the publisher can accept any legal responsibility for any errors or omissions that may be made. The publisher makes no warranty, express or implied, with respect to the material contained herein.
TNHJ also supports open access archiving of articles published in the journal after three months of publication. Authors are permitted and encouraged to post their work online (e.g, in institutional repositories or on their website) within the stated period, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See The Effect of Open Access). All requests for permission for open access archiving outside this period should be sent to the editor via email to editor@tnhjph.com.
How to Cite
References
Rose J, Chang DC, Weiser TG, Kassebaum NJ, Bickler SW. The role of surgery in global health: analysis of United States inpatient procedure frequency by condition using the Global Burden of Disease 2010 framework. PloS one. 2014 Feb 26;9(2):e89693.
Biccard BM, Madiba TE, Kluyts HL, Munlemvo DM, Madzimbamuto FD, Basenero A, Gordon CS, Youssouf C, Rakotoarison SR, Gobin V, Samateh AL. Perioperative patient outcomes in the African Surgical Outcomes Study: a 7-day prospective observational cohort study. The Lancet. 2018;391(10130):1589-98.
Aliyu D, Adeleke IT, Omoniyi SO, Kolo S, Odofin OM, EssienEkaete P. Knowledge, attitude and practice of preoperative visit: a survey of Nigerian perioperative nurses. American Journal of Health Research. 2015;3(1-1):54-60.
Duggin J Nursing in the peri-operative care environment; in Koutoukidis G, and Stainton K (eds). Essential enrolled Nursing skills for person-centered care, 2017, Elsevier, Chatswood.
Mitchell M. Day surgery nurses: selection of patient preoperative information. Journal of Clinical Nursing, 2016;(26)2:225–237.
Bestable SB, Grambert P, Jacobs K, Sopczy, K. Health Professionals as Educators: Principles of teaching and learning. 2011, Sudbury, MA: Jones & Barlet Learning, LLC
Glaysher MA, Cresswell AB. Management of common surgical complications. Surgery (Oxford). 2014 Mar 1;32(3):121-5.
Cook, DJ, et al. Patient education self-management during surgical recovery: combining mobile (iPad) and a content management system. Telemed J E Health, 2014;20(4): 312-317.
Cook DJ, Moradkhani A, Douglas KS, Prinsen SK, Fischer EN, Schroeder DR. Patient education self-management during surgical recovery: combining mobile (iPad) and a content management system. Telemedicine and e-Health. 2014;20(4):312-7.
Elkalashy, R. A. E. G. and S. E. Masry. The Effect of Preoperative Educational Intervention on Preoperative Anxiety and Postoperative Outcomes in Patients Undergoing Open Cholecystectomy. IOSR Journal of Nursing and Health Science, 2019;7(5):78-87.
Lee CK, Lee IF. Preoperative patient teaching: the practice and perceptions among surgical ward nurses. Journal of clinical nursing. 2013;22(17-18):2551-61.
Malley A, Kenner C, Kim T, Blakeney B. The role of the nurse and the preoperative assessment in patient transitions. AORN journal. 2015;102(2):181-e1.
Oyetunde, M. O, Akinneye, A. J. Factors Influencing Practice of Patient Education among Nurses at the University College Hospital, Ibadan. Open Journal of Nursing, 2015;5(5):500–507.
Ortiz J, Wang S, Elayda MA, Tolpin DA. Preoperative patient education: can we improve satisfaction and reduce anxiety? Revista brasileira de anestesiologia. 2015;65(1):7-13.
Bazezew AM, Nuru N, Demssie TG, Ayele DG. Knowledge, practice, and associated factors of preoperative patient teaching among surgical unit nurses, at Northwest Amhara Comprehensive Specialized Referral Hospitals, Northwest Ethiopia, 2022. BMC nursing. 2023;22(1):20.