Donors’ Satisfaction with Blood Donation Process and Evaluation of the Impact on their Intention to Return for Future Donations
Main Article Content
Abstract
Background: The satisfaction of blood donors with the blood donation process is crucial to their recruitment and retention. This was done to determine if there is any association between the overall satisfaction of donors with the donation process and donor demographics as well as the motivating factors and barriers to future blood donation by the donors.
Method: Information on socio-demography, blood donation history of donors, frequency of blood donation by repeat donors, rating of the donation process, level of satisfaction with the process, motivating factors and barriers to future blood donation among other data were obtained from the donors through self-administered questionnaires. Data were analyzed using SPSS for Windows version 23.0. Significant level was set at P < 0.05.
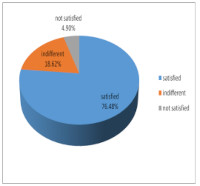
Result: Majority of the donors were within the age group of 21-30years. Their mean age was 26.54 6.68years. Seventy-six percent of the respondents expressed satisfaction with the entire blood donation process. First-time donors and males were more satisfied with the process than repeat donors and females, respectively. There was a statistically significant association between donors’ satisfaction with their intention to donate in future (p=0.032). However, the association between donors’ satisfaction, their intention to return for future donations and donors’ demographics were not statistically significant (p>0.05). Altruism was the major motivating factor while fear of needles was cited as the main barrier to future blood donations.
Conclusion: Blood donors’ satisfaction varies among demographic subgroups and is positively associated with their intention to return for future donations.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Journal is owned, published and copyrighted by the Nigerian Medical Association, River state Branch. The copyright of papers published are vested in the journal and the publisher. In line with our open access policy and the Creative Commons Attribution License policy authors are allowed to share their work with an acknowledgement of the work's authorship and initial publication in this journal.
This is an open access journal which means that all content is freely available without charge to the user or his/her institution. Users are allowed to read, download, copy, distribute, print, search, or link to the full texts of the articles in this journal without asking prior permission from the publisher or the author.
The use of general descriptive names, trade names, trademarks, and so forth in this publication, even if not specifically identified, does not imply that these names are not protected by the relevant laws and regulations. While the advice and information in this journal are believed to be true and accurate on the date of its going to press, neither the authors, the editors, nor the publisher can accept any legal responsibility for any errors or omissions that may be made. The publisher makes no warranty, express or implied, with respect to the material contained herein.
TNHJ also supports open access archiving of articles published in the journal after three months of publication. Authors are permitted and encouraged to post their work online (e.g, in institutional repositories or on their website) within the stated period, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See The Effect of Open Access). All requests for permission for open access archiving outside this period should be sent to the editor via email to editor@tnhjph.com.
How to Cite
References
Blaise NY, Exploring trends, challenges and issues of blood donation in Yaounde- Cameroon. International Journal of Biological and Pharmaceutical Sciences Archive 2022; 4: 88-98.
WHO. Blood safety and availability. Geneva; 2022. Available from https://www.who.int/news-room/fact-sheets/detail/blood-safety-and-availability.
Akpan IS, King EO, Bassey El, Umotong SJ, Nnenna WO. Assessment of the knowledge, Perception and Practice Voluntary Blood Donation among Physicians in a Tertiary Health Facility, Uyo, South-South Nigeria. Nigerian Medical Journal 2021; 62:212-218.
World Health Organization. Blood safety fact and figures 2011. Available online: www. Euro.who.int/en/what-we-do/health-topics/healthsystems/blood safety/facts-and-figures. Accessed January 2015.
Akpan IS, EkongNk, Afia RI, Uboh EE. Evaluation of Knowledge, Attitude and Practice of Volunatry Blood Donation among Healthcare Support Staff of a Tertiary Health Facility in Uyo, Nigeria. Asian Journal of Medicine and Health 2022; 20:43-53.
Nguyen DD, Devita DA, Hirschler NV, Murphy El. Blood donor satisfaction and intention of future donation. Transfusion 2008; 48: 742-748.
Weidmann C, Derstroff M, Kluter H, Oesterer M, Muller-Steinhardt M. Motivation blood donor satisfaction and intention to return during the COVID-19 pandemic. Vox Sanguinis 2021, 117:1-7.
Merxz E-M, Zijlstra BJ, Kort WL. Blood donor show behavior after an invitation to donate: the influence of collection site factors. Vox Sang uinis 2917; 112:628-37.
Melian-Alzola L, Martin-Santana JD. Service quality in blood donation: satisfaction, trust and loyalty. Service Business 2020; 14:101-29.
Ahmed N, Kumar SR. A guide to organizing a voluntary blood donation camp. International Journal of blood transfusion and Immunohematology 2013; 3:12-17.
The Melbourne declaration on 100% voluntary non-remunerated donation of blood and blood components. Composed at World Blood Donor Day. Melbourne, Australia; 2009.
Lattimore S, Wickenden C, Brailsford SR. Blood donors in England and North Wales: Demography and patterns of donation. Transfusion 2015; 55: 91-99.
Schreiber GB, Sharma UK, Wright DJ, Glynn SA, Own by HE, TU Y, et al. First year donation patterns predict long term commitment for first time donors. Vox Sanguinis 2005; 88:114-121.
De Fatima Lourencon A, des Santos Almeida R, Ferreira O, Martinez ED. Evaluation of the return rate of volunteer donors. Rev Bras HematolHemoter 2011; 33:190-4.
Akpan IS, Ino-Ekanem MB. Trends in the Seroprevalence of Transfusion-Transmissible Infections among potential Blood Donors in a Tertiary Health Facility South-South Nigeria. European Journal of Pharmaceutical and Medical Research 2017, 4:26-33.
Akpan IS, Essien EM. ABO Blood Group status and von Willebrand Factor Antigen Levels in a Cohort 100 Blood Donors in an African Population. International Journal of Biomedical Research 2016; 4:219-222.
Ogbenna A, Adewoyin A, Famuyiwa CO. Pattern of Blood Donation and Transfusion Transmissible Infections in a Hospital-based Blood Transfusion service in Lagos, Nigeria. West African Journal of Medicine 2021; 38:1088-1094.
Ugwu NI, Ugwu CN, Oti WJ, Uneke CJ. Pattern of Blood Donation Practices among students of a Nigerian University. International Blood Research and Reviews 2019; 9:1-8
Andade Neto JL, Pintarelli VL, Flechner PC, de Morais RL, Nishimoto FL. HIV prevalence among blood donors in a blood bank in Curitiba (Brazil). Brazilian Journal of Infectious Disease 2002; 69:15-21.
Ogundeyi SP, Ayayi OD, Busari OE, Ogundey OA, Adepoju OA, Esan FG. Knowledge, attitude and perception towards voluntary blood donation among University students in Nigeria. International Society of Blood Transfusion Science Series 2021; 16:85-91.
Tagny CT, Diarra A, Yahaya R, Hakizimaha M, Nguessan A, Mbensa G, et al. Characteristics of blood donors and donated blood in sub-Saharan Francophone Africa Transfusion 2009; 49:1592-99.
Saberton P, Paez A, Newbolt KB, Heddle NM. Geographical variations in the correlates of blood donor turn out rates: an investigation of Canadian metropolitan areas. Int J Health Geogr 2009; 8:56.
Ekwere TA, Ekanem MB, Ekanem AM. Assessment of Donor satisfaction with the blood Donation Process during blood Drive Campaigns and their intention to return for future Donations. World Journal of Biomedical Research 2015, 2: 27-34.
Erhabor O, Isaac Z, Abdulrahaman Y, Ndakotsu DB, Agbede F. Female gender participation in the blood donation process in resource poor settings: Case study of Sokoto in North Western Nigeria. Journal of Blood Disorders and Transfusion 2014; 5:1-5.
Nilsson SB, Sojka P. The blood donation experience: Perceived physical, Psychological and social impact of blood donation on the donor. Vox Sanguins 2003; 84:120-128.
Healy K. Embedded Altruism: blood collection regimens and the European’s donor 2000; 105: 1633-57.
Steele WR, Schreiber GB, Guilltinan A. Role of altruistic behavior, empathetic concern and social responsibility motivation in blood donation behavior. Transfusion 2008; 48; 43-54.
Rimmel M, Lattacher H, Janda M. Voluntary whole blood donation and compensated platelet donor and plasma donors: motivation to donate altruism and aggression. Transfusion and Apheresis Science 2005; 33: 147-155.
Glynn SA, Kleinma SH, Schreiber GB, Zuck T, Combs SM, Bethel J, Garratty G, Williams AE. Retrovirus Epidemiology Donor Study. Motivations to donate blood: demographic comparisons. Transfusion 2002; 42: 216-25.
Sadler A, Shi L, Bethge S, Muhlbacher A. Incentives for Blood Donation: A Discrete Choice Experiment to Analyze Extrinsic motivation. Transfusion medicine and Hemotherapy 2018:45:116-124.
United Kingdom National blood Service. A better experience all round. Available online:www.blood.co.uk/…donor/…modernism g-th. Accessed February 2015.
Kolins J, Herron R. On bowling alone and donor recruitment: lessons to be learned. Transfusion 2003; 3 1634-38.
Akpan IS, Essien EM. Measurement of von Willebrand Factor Antigen Levels in a Nigerian Population: Relative Effects of ABO Blood Group, Age, Gender and Ethnic Differences. International Journal of Science and Research Methodology 2017; 8:59-69.
France JL, France CR, Himawan LK. A path analysis of intention to redonate among experienced blood donors: an extension of the theory of planned behavior. Transfusion. 2007; 47:1006–13.
Glynn SA, Schreiber GB, Murphy EL, Kessler D, Higgins M, Wright DJ, Mathew S, Tu Y, King M, Smith JW. Retrovirus Epidemiology Donor Study. Factors influencing the decision to donate: racial and ethnic comparisons. Transfusion. 2006; 46:980–90.
Glynn SA, Williams AE, Nass CC, Bethel J, Kessler D, Scott EP, Fridey J, Kleinman SH, Schreiber GB. Retrovirus Epidemiology Donor Study. Attitudes toward blood donation incentives in the United States: implications for donor recruitment. Transfusion. 2003; 43:7–16.
PiliavinJA, Callero PL. Giving blood: the development of an altruistic identity. The Johns Hopkins University Press, Baltimore and London (1991)