Ultrasound Evaluation of Thyroid Abnormalities at the University of Port Harcourt Teaching Hospital
Main Article Content
Abstract
Background: Diseases of thyroid gland are diverse and present with varied patterns in ultrasound scan. In some cases the patterns are overlapping, making it difficult to distinguish the lesions and reach a definitive diagnosis.
Objectives: The study analysed the sonographic features of common thyroid lesions in our environment with the aim of providing a guide to sonographic diagnosis.
Patients and Methods: This was a prospective analytical study of all consecutive cases with symptomatic thyroid gland lesions referred to the radiology department for ultrasound scan. The study lasted for 18 months from January 2016 to June 2017. The study was approved by the ethics committee of our institution. The data were analysed using SPSS for windows version 20.
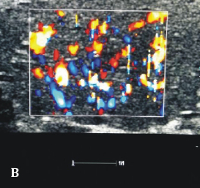
Results: There were 132 patients scanned for thyroid gland assessment during the period. Of these, 105(79.5%) were females and 27(20.5%) were males. The mean age was 34.73± 1.36years. The most common diagnosis was multinodular goitre which constituted 32 (24.24%) cases. Graves’ disease was also prevalent with a frequency of 21(15.91%) cases. Sixty patients had thyroid nodules which were of mixed echogenicity in 15 (25%) cases; hypoechogenicity in 28(46.67%) cases, hyperechogenicity in 11 (18.33%) and isoechogenicity in 6 (10%) cases. Conclusion: Thyroid abnormalities were common in our environment and were more prevalent in females. The most common lesions were multinodular goitre, Graves’ disease and Hashimoto thyroiditis. Gray scale and Doppler evaluation are of higher sensitivity in distinguishing benign from malignant nodules.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Journal is owned, published and copyrighted by the Nigerian Medical Association, River state Branch. The copyright of papers published are vested in the journal and the publisher. In line with our open access policy and the Creative Commons Attribution License policy authors are allowed to share their work with an acknowledgement of the work's authorship and initial publication in this journal.
This is an open access journal which means that all content is freely available without charge to the user or his/her institution. Users are allowed to read, download, copy, distribute, print, search, or link to the full texts of the articles in this journal without asking prior permission from the publisher or the author.
The use of general descriptive names, trade names, trademarks, and so forth in this publication, even if not specifically identified, does not imply that these names are not protected by the relevant laws and regulations. While the advice and information in this journal are believed to be true and accurate on the date of its going to press, neither the authors, the editors, nor the publisher can accept any legal responsibility for any errors or omissions that may be made. The publisher makes no warranty, express or implied, with respect to the material contained herein.
TNHJ also supports open access archiving of articles published in the journal after three months of publication. Authors are permitted and encouraged to post their work online (e.g, in institutional repositories or on their website) within the stated period, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See The Effect of Open Access). All requests for permission for open access archiving outside this period should be sent to the editor via email to editor@tnhjph.com.
How to Cite
References
Suwadi MA, Tabari AM, Isyaku K, Idris SK, Saleh MK, Abdulkair AY. Sonographic measurement of normal thyroid gland volume in school children in Kano, Nigeria. West African Journal of Ultrasound 2008; 8: 14- 21
Ahijo A, Tahir A, Tukur MA. Ultrasound determination of thyroid gland volume among adult Nigerians. The Internet Journal of Radiology 2006; 4:1-3.
Azizi F, Malic M, Bebers E, Delshad H, Bakir A. Thyroid volumes in school children of the Emirates. J Endocrinol Invest 2003; 26: 56-60.
Alper O, Sukru ME, Alkin E et al. The diagnostic efficiency of ultrasound in characterization for thyroid nodules: how many criteria are required to predict malignancy? Medical Ultrasonography 2012; 14(1): 24-28.
Solbiati L, Charboneau JW, Osti V, James EM, Hay ID. The thyroid gland. In: Rumack CM, Wilson SR, Charboneau JW, editors. Diagnostic Ultrasound. 3rd ed. Vol. 1. St. Louis, Missouri: Elsevier Mosby; 2005. pp. 735–70.
Chaudhary V, Bano S. Imaging of the thyroid: Recent advances. Indian J Endocrinol Metab. 2012; 16:371–6. [PMCID: PMC3354842] [PubMed: 22629501]
Nelson M, Wickus GG, Caplan RH, Begium EA. Thyroid gland size in pregnancy. An ultrasound and clinical study. J Reprod Med 1987; 32(12): 888-90
Rasmussen NG, H.orness PJ, Hegedus L. Ultrasonographically determined thyroid size in pregnancy: Postpartum: the goitrogenic effect of pregnancy. Am J Obstet Gynecol 1989; 160(9): 1216-20.
Iko BO. Grey scale ultrasonography of the thyroid gland, Nigeria. Trop Geogr Med. 1986; 38(1): 21-7.
Li RQ, Yuan GH, Chen M, Shao YM, Zhu SN, Zhang JQ, Guo XH. Evaluation of Diagnostic Efficiency of Ultrasound Features on Malignant Thyroid Nodules in Chinese Patients. Chin Med J 2016; 129:1784-8.
Kocak M, Erem C, Deger O, Topbas M, Ersoz HO, Can E. Current prevalence of goiter determined by ultrasonography and associated risk factors in a formerly iodine – deficient area of Turkey. Endocrine 2014; 47: 290 8. dio: 10.1007/s12020-013-0153-2.
Babcock DS. Thyroid disease in the pediatric patients: emphasizing imaging with sonography. Pediatric Radiol 2006; 36: 299-304
Farwell AP, Braverman LE. Inflammatory thyroid disorders. Otolaryngol Clin North Am 1996; 29: 541-556.
Manjiri D, Richard B, Jorg B, Vito C, Maria CC, David C et al. Thyroid ultrasound: state of the art. Part1- thyroid ultrasound reporting and diffuse thyroid diseases. Med Ultrason 2017; 19(1): 79-93: Doi: 10.1111m-980
Fathimabeebi PK, Noor BA, Hilal NA, Sulaiman ZA. The prevalence of thyroid cancer in patients with hyperthyroidism. Saudi Med J 2015; 36(7): 874-877a. Doi: 10.15537/smj.2015.7.11463.
Hegedus L, Bonnema SJ, Bennedbaek FN. Management of simple nodular goiter: current status and future perspectives. Endocr Rev 2003;24:102-132.
Rago T, Santini F, Scutari M, Pinchera A, Vitti P. Elastography: new developments in ultrasound for predicting malignancy in thyroid nodules. J Clin Endocrinol Metab.2007; 92: 2917-22.
Alpana Manchanda. Thyroid imaging. In: Niranjan K, Veena C, Arun KG, editors. Diagnostic Radiology, neuroradiology including head and neck imaging. 3rd edn. India, JPBMP, 2010; 421-447.
Vikas C, Shahina B. Thyroid ultrasound. Indian J Endocrinol Metab. 2013; 17(2): 219-227. dio 10.4103/2230-8210.109667.
Castagnone D, Rivolta B, Rescalli S, et al. Colour Doppler sonography in Graves’ disease: Value in assessing activity of disease and predicting outcome. AJR 1996; 66:203-07
Pishdad P, Pishdad GR, Tavanaa S, Pishdad R, Jalli R. Thyroid Ultrasonography in Differentiation between Graves’ Disease and Hashimoto’s Thyroiditis. J Biomed Phys Eng. 2017; 7(1): 21-26
Anderson L, Middleton WD, Teefey SA et al. Hashimoto’s thyroiditis: Part 1, sonographic analysis of the nodular form of Hashimoto thyroiditis. AJR 2010; 195: 208-115.
Moon WJ, Jung SL, Leeh JH et al. Benign and malignant thyroid nodules: Ultrasound differentiation-multicenter retrospective study. Radiology 2008; 247: 762-770.
Uliaque CF, Berdún FJP, Herrero RL, Lórenz CP. Usefulness of ultrasonography is the evaluation of thyroid nodules. Radiologia 2016; 58: 380-388
Bonavita JA, Mayo J, Babb J, Bennett G, Macar M, et al. Pattern recognition of benign nodules at ultrasound of the thyroid: which nodules can be left alone? AJR 2009; 193: 2017-13