Outcome of Active and Physiological Management of Third Stage of Labour in a Tertiary Hospital in Aba, Abia State.
Main Article Content
Abstract
Background: Active management of third stage of labour involves giving prophylactic uterotonic agents, early cord clamping and cutting and, the use of controlled-cord-traction to deliver the placenta, while the physiological management of third stage of labour is a natural process that occurs following the end of the second stage of labour. This aim is to assess outcome of third stage of labour management outcome between active and physiological management during vaginal delivery.
Method: The study was a cross-sectional comparative analytic survey research design. The sample size is 200 participants comprising 150 midwives and 50 doctors, obtained through census sampling. Data was collected using self-structured questionnaire. Data analysis was done using SPSS.
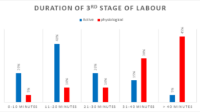
Findings: About 65% of the respondents utilized active method while 35% of the respondents utilized physiological method. Outcome of physiological method revealed that 55% of the respondents never encounter uterine inversion and accidental cutting of the umbilical cord while the placenta is still in-utero respectively. 55% respondents expressed that retained placenta and blood loss is always expected in this method. 60% of respondents always encounter PPH while managing their patients on physiologic method.
Conclusion: The outcome of physiological method includes prolonged third stage period, retained placenta and increased blood loss, while the outcome of active method includes short period of third stage of labour, decreased blood loss, uterine inversion, accidental cutting of umbilical cord.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
The Journal is owned, published and copyrighted by the Nigerian Medical Association, River state Branch. The copyright of papers published are vested in the journal and the publisher. In line with our open access policy and the Creative Commons Attribution License policy authors are allowed to share their work with an acknowledgement of the work's authorship and initial publication in this journal.
This is an open access journal which means that all content is freely available without charge to the user or his/her institution. Users are allowed to read, download, copy, distribute, print, search, or link to the full texts of the articles in this journal without asking prior permission from the publisher or the author.
The use of general descriptive names, trade names, trademarks, and so forth in this publication, even if not specifically identified, does not imply that these names are not protected by the relevant laws and regulations. While the advice and information in this journal are believed to be true and accurate on the date of its going to press, neither the authors, the editors, nor the publisher can accept any legal responsibility for any errors or omissions that may be made. The publisher makes no warranty, express or implied, with respect to the material contained herein.
TNHJ also supports open access archiving of articles published in the journal after three months of publication. Authors are permitted and encouraged to post their work online (e.g, in institutional repositories or on their website) within the stated period, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See The Effect of Open Access). All requests for permission for open access archiving outside this period should be sent to the editor via email to editor@tnhjph.com.
How to Cite
References
NICE Prevention and Management of Post-Partum Haemorrhage. An International Journal of Obstetrics and Gynaecology. 2017; 124. (5):P.e106e149, https://doi.org/10.1111/1471-0528.14178
Smith JR, Brennan BG . Management of the third stage of labor. E-medicine. http://www.emedicine.com/med/topic3569.htm
Oladapo OT, Okusanya BO, Abalos E, Gallos ID, Papodopoulou A. Intravenous versus intramuscular prophylactic oxytocin for the third stage of labour. Cochrane Database Syst Rev. 2020;(3). DOI: 10.1002/14651858.CD009332.pub4
Donald I. Postpartum haemorrhage. In: Practical obstetric problems. London: Lloyd-Luke. 2023; 748–94.
Farrar, D, Tuffnel lD, Airey, R. Care During the Third Stage of Labour. A postal Survey of UK Midwives and Obstetricians. BMC Pregnancy Childbirth 10.23 (2019). https://doi.org/10.1186/147-2393-10–23.
Kumar, N, Jahanfar, S, Haas, M & Weeks, AD. Umbilical vein injection for management of retained placenta. The Cochrane Database of Systematic Reviews, 3(3), CD001337. https://doi.org/10.1002/14651858.CD001337.pub3
Mousa, HA., Blum, J, Abou E, Senoun, G, Shakur, H & Alfirevic, Z. Treatment for primary postpartum haemorrhage. The Cochrane Database of Systematic Reviews, 2, CD003249. DOI: 10.1002/14651858.CD003249.pub3
Begley CM, Gyte GML, Weeks A. Active versus physiological management for women in the third stage of labour [Internet]. 2014 [cited 2025 Sep 11]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles
Zhu C, Estrade M, White J, Lal M. Heat-stable sublingual oxytocin tablets as a potential needlefree approach for preventing postpartum haemorrhage in low-resource settings. Drug Deliv Transl Res. 2018; 8:853–6. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles
Begley, CM, Gyte, GML, Devane, D & Mcguire, W Active Versus Physiological Management for
Women in the Third Stage of Labour. Cochrane Database System 9: (ii): CD007412. doi: 10 – 1002/ 14651858.
World Health Organization. WHO guideline for the management of postpartum haemorrhage and retained placenta. Geneva: WHO; 2019. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles
Royal College of Obstetrist and Gynaecologist. Prevention and Management of Postpartum
Haemorrhage, An International Journal of Obstetrics and Gynaecology longing/volume 124, issue5/p.e106-2149.Green-top Guideline No52.https://doi.org/10.1111/1471-0528.141178
McDonnld, SJ, Middleton, P & Dowswell, T. Effect of Timing of Umblical Cord Clamping of Term Infants on Maternal and Neonatal Outcomes. Evidenced Based Child Health. 2014 June 9 (2):303-97
Gulmezoglu, AM, Widmer, M, Merialdi, M, Qureshi, Z, Piagglo, G & Elbourne, M. Active
Management of Third Stage of LabourWithout Controlled cord Traction a randomized noninferiority-controlled Trial of Reproductive Health. Retrieved from www.ncbi.n/m.nih.gov/pem/article.
Elbourna, DR, Prendiville, WJ, Carroli, G. Prooophylactic Use of Oxytocine in the Third
Dixon L, Thompson S, Guilliland K, Pairman S, Lennox S, Tracy S, et al. Midwives’ care during the third stage of labour: an analysis of the New Zealand College of Midwives 2019;35:18–23 Midwifery Database 2019. www.ncbi.n/m.nh.goo/pcm/aitide.
Burke TF, Ahn R, Nelson BD, Hines R, Kamara J. A postpartum haemorrhage package with Condom Uterine Balloon Tamponade: A Prospective Multicentre case series in Kenya, Sierra Leone, Senegal, and Nepal. BJOG. 2016;123(9):1532–40.
Buckley SJ. Executive summary of hormonal physiology of childbearing: evidence and implications for women, babies, and maternity care. J Perinat Educ. 2015;24(3):145–53.
Fry JL, Dombrowski MP. Postpartum hemorrhage and the role of uterine tamponade. Obstet Gynecol Clin North Am. 2017;44(1):95–106.
Cernadas JMC. Prevention of postpartum haemorrhage in low-resource settings. Int J Gynaecol Obstet. 2016;134(3):267–70
Chaparro CM, Lutter CK. Increases in breastfeeding duration observed in Latin America and the Caribbean from 1990 to 2010. The Journal of Nutrition, 146(10), 1888-1895.
McDonald SJ, Middleton P. Effect of timing of umbilical cord clamping of term infants on maternal and neonatal outcomes. The Cochrane Database of Systematic Reviews, (7), CD004074. https://doi.org/10.1002/ebch.1971
Van Rheenen, PF & Brabin, BJ. A practical approach to timing cord clamping in resource poor settings. BMJ, 358, j2740. doi: https://doi.org/10.1136/bmj.39002.389236.BE