Child Nutritional status and Practice of C-IMCI among Mothers in Urban and Rural Communities in Oyo state
Main Article Content
Abstract
Background: The introduction of the community component of the integrated management of childhood illnesses, (C-IMCI) includes the development of key household practices (KHPs) and has led to better health outcomes among under-five children. However, malnutrition and childhood illnesses continue to linger among under-five children across communities in Nigeria. This study comparatively explores the knowledge and adoption of key household practices as well as childhood nutritional status in selected rural and urban areas in Oyo state, Nigeria.
Method: A comparative cross-sectional study conducted in Ibadan Northeast and Akinyele local government areas of Oyo State. A total of 484 children aged 0-59 months and their mothers/caregivers were assessed using an interviewer-administered questionnaire adapted from the UNICEF Multiple Indicator Cluster Survey and Nigerian National Demographic and Health Survey tools.
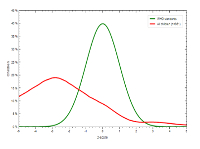
Result: Mean age of mothers was 29.8+5.60 and slightly above half of the urban dwellers (56.4%) had good knowledge of child psychosocial development while half of the rural dwellers had poor knowledge (51.7%). More urban (64.4%) than rural (56.4%) dwellers had good composite key household practices (KHPs) (p=0.011). Stunting (64.1%) was the most prevalent type of malnutrition, and there were more wasted and underweight children in urban areas (12.0% and 23.4%) than in rural areas (8.5% and 22.0%).
Conclusion: The observed gaps in practice of KHPs and nutritional status of under-fives in urban and rural communities calls for greater awareness on key household practices through tailored health campaigns. This should be directed at communities to improve the knowledge and practice of KHPs among caregivers.
Downloads
Article Details
Issue
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Journal is owned, published and copyrighted by the Nigerian Medical Association, River state Branch. The copyright of papers published are vested in the journal and the publisher. In line with our open access policy and the Creative Commons Attribution License policy authors are allowed to share their work with an acknowledgement of the work's authorship and initial publication in this journal.
This is an open access journal which means that all content is freely available without charge to the user or his/her institution. Users are allowed to read, download, copy, distribute, print, search, or link to the full texts of the articles in this journal without asking prior permission from the publisher or the author.
The use of general descriptive names, trade names, trademarks, and so forth in this publication, even if not specifically identified, does not imply that these names are not protected by the relevant laws and regulations. While the advice and information in this journal are believed to be true and accurate on the date of its going to press, neither the authors, the editors, nor the publisher can accept any legal responsibility for any errors or omissions that may be made. The publisher makes no warranty, express or implied, with respect to the material contained herein.
TNHJ also supports open access archiving of articles published in the journal after three months of publication. Authors are permitted and encouraged to post their work online (e.g, in institutional repositories or on their website) within the stated period, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See The Effect of Open Access). All requests for permission for open access archiving outside this period should be sent to the editor via email to editor@tnhjph.com.
How to Cite
References
IMCI Integrated Management of Childhood Illness. World Health Organization UNICEF; 2005.
Ajmal A, White F, Younus M, Kadir M, Ali S, Fatmi Z. Eight key household practices of Integrated Management of Childhood Illnesses (IMCI) amongst mothers of children aged 6 to 59 monthsin Gambat, Sindh, Pakistan. JPMA The Journal of the Pakistan Medical Association. 2007;57:288-93.
Winch PJ, Leban K, Casazza L, Walker L, Pearcy K. An implementation framework for household and community integrated management of childhood illness. Health Policy Plan. 2002;17(4):345-53. [DOI: 10.1093/heapol/17.4.345]
Ifeanyichukwu OA, Ossaidiom OV, Obehi OH. Nutritional status of under-five children in urban and rural communities of Edo State, Nigeria. Ibom Medical Journal. 2018 Aug 1;11(2):31-43.
Fatiregun FA, Adejugbagbe AM. Nutritional status of under-fives in rural and urban communities of Southwest, Nigeria. World Academic Journal of Community Health and Epidemiologyealth and Epidemiology. 2016 Apr;2(4):064-73.
Senbanjo IO, Olayiwola IO, Afolabi WA. Dietary practices and nutritional status of under-five children in rural and urban communities of Lagos State, Nigeria. Nigerian Medical Journal: Journal of the Nigeria Medical Association. 2016 Nov;57(6):307.
Children: Improving Survival and Well-being. World Health Organization; 2020. Available from: www.who.int.
‘Levels & Trends in Child Mortality: Report 2020, Estimates developed by the United Nations Inter-agency Group for Child Mortality Estimation’. New York: United Nations Children’s Fund; 2020.
Findley SE, Uwemedimo OT, Doctor HV, Green C, Adamu F, Afenyadu GY. Early results of an integrated maternal, newborn, and child health program, Northern Nigeria, 2009 to 2011. BMC Public Health. 2013;13:1034-. [DOI: 10.1186/1471-2458-13-1034]
Ogaji DS, Arthur AO, George I. Effectiveness of Mobile Phone-Based Support on Exclusive BreastfeeA Randomized Controlled Trial. J Trop Pediatr. 2021;67(1). [DOI:10.1093/tropej/fmaa076]
Obasola OI, Mabawonku I, Lagunju I. A Review of e-Health Interventions for Maternal and Child Health in Sub-Sahara Africa. Matern Child Health J. 2015;19(8):1813-24. [DOI: 10.1007/s10995-015-1695-0]
Adekanmbi VT, Kayode GA,Uthman OA. Individual and contextual factors associated with childhood stunting in Nigeria: a multilevel analysis. Maternal & Child Nutrition. 2013;9(2):244-59. [DOI: https://doi.org/10.1111/j.1740-8709.2011.00361.x]
Nutrition and Health Survey (NNHS) 2018. Nigeria: National Bureau of Statistics (NBS), National Population Commission (NPopC), Nigeria Federal Ministry of Health, United Nations Children's Fund (UNICEF); 2018.
Nutrition. UNICEF. Available from: www.unicef.org. assessed on 22/11/2021
Goal 3: Ensure healthy lives and promote well-being for all at all ages. United Nations. Available from: sdgs.un.org.
Improving Child Nutrition-The achievable imperative for global progress. United Nations Children’s Fund (UNICEF); 2013.
Li Z, Kim R, Vollmer S, Subramanian SV. Factors Associated With Child Stunting, Wasting, and Underweight in 35 Low-and Middle-Income Countries. JAMA Netw Open. 2020;3(4):e203386-e. [DOI: 10.1001/jamanetworkopen.2020.3386]
Danaei G, Andrews KG, Sudfeld CR, Fink G, McCoy DC, Peet E, et al. Risk Factors for Childhood Stunting in 137 Developing Countries: A Comparative Risk Assessment Analysis at Global, Regional, and Country Levels. PLoS Med. 2016;13(11):e1002164. [DOI: 10.1371/journal.pmed.1002164]
Fadairo O. and Orifah M. Adherence to Selected Key Household Practices for Child Survival among Rural Women in Etche Local Government Area of Rivers State. Journal of Agricultural Economics, Extension & Social Sciences. 2018; 1(2):19-27.
Kirkwood BR. Essentials of Medical Statistics. In: Essentials of Medical Statistics Essentials of Medical Statistics. 2nd ed: Blackwell Scientific Publications; 1988.
National Bureau of Statistics. Nigeria Multiple Indicator Cluster Survey. 2011.]
Thompson ME, Harutyunyan TL. Impact of a community-based integrated management of childhood illnesses (IMCI) programme in Gegharkunik, Armenia. Health Policy Plan. 2009;24(2):101-7. [DOI: 10.1093/heapol/czn048]
Mukunya D, Kizito S, Orach T, Ndagire R, Tumwakire E, Rukundo GZ, et al. Knowledge of integrated management of childhood illnesses community and family practices (C-IMCI) and association with child undernutrition in Northern Uganda: a cross-sectional study. BMC Public Health. 2014;14:976-. [DOI: 10.1186/1471-2458-14-976]
Leonard T, Hughes AE, Pruitt SL. Understanding how low-socioeconomic status households cope with health shocks: An analysis of multi-sector linked data. Ann Am Acad Pol Soc Sci. 2017;669(1):125-45. [DOI: 10.1177/0002716216680989]
Arifeen SE, Hoque DM, Akter T, Rahman M, Hoque ME, BegumK, et al. Effect of the Integrated Management of Childhood Illness strategy on childhood mortality and nutrition in a rural area in Bangladesh: a cluster randomised trial. Lancet. 2009;374(9687):393-403. [DOI: 10.1016/s0140-6736(09)60828-x]
Martins VJ, Toledo Florêncio TM, Grillo LP, Franco MD, Martins PA, Clemente AP, Santos CD, Vieira MD, Sawaya AL. Long-lasting effects of undernutrition. International journal of environmental research and public health. 2011 Jun;8(6):1817-46.
Tesfaw LM, Fenta HM. Multivariate logistic regression analysis on the association between anthropometric indicators of under-five children in Nigeria: NDHS 2018. BMC Pediatr. 2021;21(1):193. [DOI: 10.1186/s12887-021-02657-5]
Harding KL, Aguayo VM, Webb P. Factors associated with wasting among children under five years old in South Asia: Implications for action. PLoS One. 2018;13(7):e0198749-e. [DOI: 10.1371/journal.pone.0198749]
Demissie S, Worku A. Magnitude and factors associated with malnutrition in children 6-59 months of age in pastoral community of Dollo Ado district, Somali region, Ethiopia. Sci J Public Health. 2013;1(4):175-83.]
Khan S, Zaheer S, Safdar NF. Determinants of stunting, underweight and wasting among children <5years of age: evidence from 2012-2013 Pakistan demographic and health survey. BMC Public Health. 2019;19(1):358. [DOI: 10.1186/s12889-019-6688-2]
Levels and trends in child malnutrition: Key Findings of the 2020 Edition of the Joint Child Malnutrition Estimates. Geneva: United Nations Children’s Fund (UNICEF), World Health Organization, International Bank for Reconstruction and Development/The World Bank; 2020.
Walson JL, Berkley JA. The impact of malnutrition on childhood infections. Curr Opin Infect ding and Infant Growth in Nigeria: Dis. 2018;31(3):231-6. [DOI: 10.1097/QCO.0000000000000448]
Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382(9890):427-51. [DOI: 10.1016/s0140-6736(13)60937-x]
Owoaje E, Onifade O, Desmennu A. Family and socioeconomic risk factors for undernutrition among children aged 6 to 23 Months in Ibadan, Nigeria. Pan Afr Med J. 2014;17:161. [DOI: 10.11604/pamj.2014.17.161.2389]
Tette EMA, Sifah EK, Nartey ET. Factors affecting malnutrition in children and the uptake of interventions to prevent the condition. BMC Pediatr. 2015;15:189-. [DOI: 10.1186/s12887-015-0496-3]
QA A. An Assessment of the Who/Unicef Key Household Practices In Edo State, Nigeria. University of Benin Teaching Hospital Benin City, Edo State: National Postgraduate Medical College of Nigeria; 2014.
Maduforo AN, Onuoha RO. Relativities of exclusive breastfeeding between urban and rural lactating women in Imo State. Jorind. 2011;1:31-6.
Adedokun ST, Uthman OA, Adekanmbi VT, Wiysonge CS. Incomplete childhood immunization in Nigeria: a multilevel analysis of individual and contextual factors. BMC Public Health. 2017;17(1):236. [DOI: 10.1186/s12889-017-4137-7]
Singh PK. Trends in child immunization across geographical regions in India: focus on urban-rural and gender differentials. PLoS One. 2013;8(9):e73102. [DOI: 10.1371/journal.pone.0073102]
Owais A, Hanif B, Siddiqui AR, Agha A, Zaidi AKM. Does improving maternal knowledge of vaccines impact infant immunization rates? A community-based randomized-controlled trial in Karachi, Pakistan. BMC Public Health. 2011;11(1):239. [DOI: 10.1186/1471-2458-11-239]
Sibeudu FT, Uzochukwu BS, Onwujekwe OE. Rural–urban comparison of routine immunization utilization and its determinants in communities in Anambra states, Nigeria. SAGE open medicine. 2019 Jan;7:2050312118823893.
Adesuwa Q. A. (2014). View of an assessment of the WHO/UNICEF key household practices in Edo State, Nigeria. https://www.dissertation.npmcn.edu.ng/index.php/FMCPH/article/view/2552/2354
Ajibuah, B. (2018). Evaluation of Nutritional Status of Under-5 Children in Borno and Kano States of Nigeria Ife Social Sciences Review, 26(1), 66–73.
Ali, M. S., Kassahun, C. W., & Wubneh, C. A. (2020). Overnutrition and Associated Factors: A Comparative Cross-Sectional Study between Government and Private Primary School Students in Gondar Town, Northwest Ethiopia. Journal of Nutrition and Metabolism, 2020. https://doi.org/10.1155/2020/3670895 -
El-Rufai. (2017). Malnutrition in Kaduna frightening. https://dailynigerian.com/malnutrition-in-kaduna-frightening-gov-el-rufai/
Khan, D. S. A., Das, J. K., Zareen, S., Lassi, Z. S., Salman, A., Raashid, M., Dero, A. A., Khanzada, A., & Bhutta, Z. A. (2022). Nutritional Status and Dietary Intake of School-Age Children and Early Adolescents: Systematic Review in a Developing Country and Lessons for the Global Perspective. Frontiers in Nutrition, 8, 1310. https://doi.org/10.3389/FNUT.2021.739447/BIBTEX
Ume Okonkwo, A. A., Ibekwe, M. U., Umeokonkwo, C. D., Okike, C. O., Ezeanosike, O. B., & Ibe, B. C. (2020). Nutritional status of school age children in Abakaliki metropolis, Ebonyi State, Nigeria. BMC Pediatrics, 20(1), 1–9. https://doi.org/10.1186/S12887-020-1994-5/TABLES/4
Zacchaeus Adeyanju, O., & Fadupin, G. T. (2022). Double burden of malnutrition among mothers and their under five children in rural areas of Oyo State, Nigeria. World Nutrition, 13(4), 21–28. https://doi.org/10.26596/WN.202213421-28