Healthcare workers’ perceptions of COVID-19 in four regions of Tanzania: A quantitative cross-sectional survey in healthcare facilities
Main Article Content
Abstract
Background: On 16 March 2020, the first COVID-19 case was reported from Mount Meru Hospital in Arusha region, a public hospital in northern Tanzania. Tanzanian Government ordered the closure of all schools and universities the next day, as well as the prohibition of all public gatherings except churches and mosques. This study was conducted to assess level of COVID-19 perception among healthcare workers in selected regions of Tanzania in order to strengthen healthcare system.
Methods: A quantitative analytical cross-sectional survey design was conducted from 24th of August to 3rdOctober involving 596 healthcare workers from Dar es Salaam, Mwanza, Arusha and Dodoma regions. Statistical Package for the Social Sciences (SPSS) 26 version was used to analyze collected data giving frequencies and percentages for categorical variables. Association between categorical variables were analyzed by using Chi-square and significant relationship observed at P-value < 0.05.
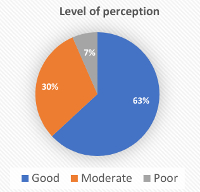
Results: Healthcare workers in the study areas had an average of 79.9% of positive perception which is moderate. About 63%, 30%, and 7% of healthcare workers holding good, moderate, and low levels of perception respectively. Four predictors (sex, field profession, level of education and region) had significant relationship with level of perception, all had P-value (P< 0.05).
Conclusion: Most of participants showed positive perception on believing that it is necessary to have regular training related to epidemics even when they do not exist and that, society can facilitate the eradication of COVID-19.
Downloads
Article Details
Issue
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Journal is owned, published and copyrighted by the Nigerian Medical Association, River state Branch. The copyright of papers published are vested in the journal and the publisher. In line with our open access policy and the Creative Commons Attribution License policy authors are allowed to share their work with an acknowledgement of the work's authorship and initial publication in this journal.
This is an open access journal which means that all content is freely available without charge to the user or his/her institution. Users are allowed to read, download, copy, distribute, print, search, or link to the full texts of the articles in this journal without asking prior permission from the publisher or the author.
The use of general descriptive names, trade names, trademarks, and so forth in this publication, even if not specifically identified, does not imply that these names are not protected by the relevant laws and regulations. While the advice and information in this journal are believed to be true and accurate on the date of its going to press, neither the authors, the editors, nor the publisher can accept any legal responsibility for any errors or omissions that may be made. The publisher makes no warranty, express or implied, with respect to the material contained herein.
TNHJ also supports open access archiving of articles published in the journal after three months of publication. Authors are permitted and encouraged to post their work online (e.g, in institutional repositories or on their website) within the stated period, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See The Effect of Open Access). All requests for permission for open access archiving outside this period should be sent to the editor via email to editor@tnhjph.com.
How to Cite
References
Le XT, Nguyen QT, Onyango B, Nguyen QN, Pham QT, Ta NT, et al. Perception toward exposure risk of COVID-19 among health workers in Vietnam: Status and correlated factors. Front Public Health. 2021; 9:589317
Mofijur M, Fattah IM, Alam MA, Saiful ABM, Ong HC, Ashrafur SM, et al. Impact of COVID-19 on the social, economic, environmental and energy domains: lessons learnt from a global pandemic. Sustain Prod Consum. (2021); 26:343–59. doi: 10.1016/j.spc.2020.10.016
World Health Organization. WHO Coronavirus (COVID-19) Dashboard. 2021. Available online at: https://covid19.who.int/(Accessed 27 February 2023).
Lua W, Hang Wang H, Yuxing Lin Y, Li L. Psychological status of medical workforceduring the COVID-19 pandemic: a cross-sectional study. Psychiatry Res. 2020; 288:112936. https://doi.org/10.1016/j.psychres.2020.112936.
Jordan RE, Adab P, Cheng K. Covid-19: risk factors for severe disease and death. Bmj. 2020;368.
Gorini S, Fiabane E, Sommaruga M, Barbieri S, Sottotetti F, La Rovere MT, et al. Mental health and risk perception among Italian healthcare workers during the second month of the Covid-19 pandemic. Arch Psychiatr Nurs. (2020) 34:537–44. doi: 10.1016/j.apnu.2020.10.007
Ran L, Chen X, Wang Y, Wu W, Zhang L, Tan X. Risk factors of healthcare workers with coronavirus disease 2019: a retrospective cohort study in a designated hospital of wuhan in China. Clin Infect Dis. 2020;71(16):2218–2221.
Vimercati L, De Maria L, QuaratoM, Caputi A, Stefanizzi P, Gesualdo L, et al. COVID-19 hospital outbreaks: Protecting healthcare workers to protect frail patients. An Italian observational cohort study. International Journal of Infectious Diseases. 2021; 102:532-7.
Bashirian S, Jenabi E, Khazaei S, Barati M, Karimi-Shahanjarini A, Zareian S, et al. Factors associated with preventive behaviours of COVID-19 among hospital staff in Iran in 2020: an application of the Protection Motivation Theory. J Hosp Infect. 2020;105(3):430-3.
World Health Organization (WHO). Risk Communication and Community Engagement (RCCE) Action Plan Guidance COVID-19 Preparedness and Response. 2020. Available from; https://www.who.int/docs/default-source/coronaviruse/covid19-rcce-guidance-final-brand.pdf. (Accessed 27 February 2023).
Nguyen LH, Drew DA, Graham MS, Joshi AD, Guo CG, Ma W, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. The Lancet Public Health. 2020; 5(9): e475-83
Verbeek JH, Rajamaki B, Ijaz S, Sauni R, Toomey E, Blackwood B, et al. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane database of systematic reviews. 2020(4).
Girma S, Agenagnew L, Beressa G, Tesfaye Y, Alenko A. Risk perception and precautionary health behavior toward COVID-19 among health professionals working in selected public university hospitals in Ethiopia. Plos one. 2020; 15(10): e0241101.
Makoni, M. Tanzania refuses COVID-19 vaccines. The Lancet. 2021. Available from; https://www.thelancet.com/journals/lancet/article/PIIS0140 6736(21)00362-7/fulltext; (Accessed 26 February 2023).
Mtani FA, Ngohengo J. Africa at the Crossroads: An Overview of theCovid-19 Pandemic and its Drama in Tanzania. African Journal of History and Geography. 2023; 2(1):1-6.
Rugarabamu S, Ibrahim M, Byanaku A. Knowledge, attitudes, and practices (KAP) towards COVID-19:
A quick online cross-sectional survey among Tanzanian residents. medRxiv. 2020; doi: https://doi.org/10.1101/2020.04.26.20080820
Munga MA, Mæstad O. Measuring inequalities in the distribution of health workers: the caseof Tanzania. Hum Resour Health. 2009;7(1):1-12.
Macrotrends Tanzania population growth rate 1950-2022. Available from: https://www.macrotrends.net/countries/TZA/tanzania/population-growth-rate. (Accessed 20 May 2022).
World population review. Available from: https://worldpopulationreview.com/world-cities/dodoma-population. (Accessed 20 May 2022).
Krejcie RV, Morgan DW. Determining sample size for research activities. Educ Psychol Meas. 1970;30(3):607-10.
Feleke BT, Wale MZ, Yirsaw MT. Knowledge, attitude and preventive practice towards COVID-19 and associated factors among outpatient service visitors at Debre Markos compressive specialized hospital,north-west Ethiopia. Plos one. 2021; 16(7): e0251708.
Abolfotouh MA, Almutairi AF, BaniMustafa AA, Hussein MA. Perception and attitude of healthcare workers in Saudi Arabia with regard to Covid-19 pandemic and potential associated predictors. BMC Infect Dis. 2020; 20:1-0.
Abolfotouh MA, AlQarni AA, Al-Ghamdi SM, Salam M, Al-Assiri MH, Balkhy HH. An assessment of the level of concern among hospital-based health-care workers regarding MERS outbreaks in Saudi Arabia. BMC Infect Dis. 2017; 17:4. https://doi.org/10.1186/s12879-016-2096-8.
Huynh TL. The COVID-19 risk perception: a survey on socioeconomics and media attention. Econ Bull. (2020) 40:758–64.
Gómez-Ochoa SA, Franco OH, Rojas LZ, Raguindin PF, Roa-Díaz ZM, Wyssmann BM, et al. COVID-19 in health-care workers: a living systematic review and meta-analysis of prevalence, risk factors, clinical characteristics, and outcomes. Am J Epidemiol. 2021; 190(1):161-75.
Simione L, Gnagnarella C. Differences between health workers and general population in risk perception, behaviors, and psychological distress related to COVID-19 spread in Italy. Front Psychol. 2020; 11:2166.
Xiong Y, Gao M, van Duijn B, Choi H, van Horssen F, Wang M. International policies and challenges on the legalization of traditional medicine/herbal medicines in the fight against COVID-19. Pharmacol. Res. 2021; 166:105472.
French Agency for Food, Environmental and Occupational Health & Safety. ANSES Warns Against Taking Food Supplements That Could Lower the Body’s Immune Response, 2020. https://www.anses.fr/fr/system/fifiles/NUT2020SA0045.pdf, (Accessed 26 February 2023).
Wildman WJ, Bulbulia J, Sosis R, Schjoedt U. Religion and the COVID-19 pandemic. Religion Brain Behav. 2020;10(2):115-7
Channel News Asia (CNA). Church at centre of South Korea COVID-19 sits silent as infections surge [Internet]. Channel News Asia, 2020. Available from: https://www.channelnewsasia.com/news/asia/coronavirus-covid19-church-south-korea-empty12458786; [Accessed 25 February 2023].
Al-Rousan N, Al-Najjar H. Is visiting Qom spread CoVID-19 epidemic in the Middle East? Eur Rev Med Pharmacol Sci. 2020; 24: 5813–5818.
Barmania S, Reiss MJ. Health promotion perspectives on the COVID-19 pandemic: The importance of religion. Glob Health Promot. 2021; 28(1):15-22.
Che Mat NF, Edinur HA, Abdul Razab MK, Safuan S. A single mass gathering resulted in massive transmission of COVID-19 infections in Malaysia with further international spread. J Travel Med. 2020; 27(3): taaa059.
Mol MP, Caldas S. Can the human coronavirus epidemic also spread through solid waste? Waste Manag Res. 2020; 38(5):485-6.
Donno DR, Grattagliano I, Rossi A, Lora Aprile P, Medea G, LagolioE, et al. How to treat COVID-19 patients at home in the Italian context: an expert opinion. Infect Dis Rep. 2021;13(1):251-8.