Self-Medication with Over-the-Counter Drugs in Children: Examining the Common Medications and Factors Influencing Mothers' Choices
Main Article Content
Abstract
Background: Self-medication with over-the-counter (OTC) drugs among children is widespread and crosses socioeconomic lines. Although OTC drugs offer convenience, their unregulated use can pose health risks, especially to children. Understanding these risks and the factors influencing self-medication practices is crucial for developing safer medication approaches. The aim of this study is to assess the attitudes and practices of mothers toward self-medication with OTC drugs for their children in Awka, Anambra State, Nigeria.
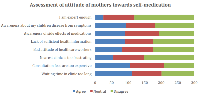
Method: A cross-sectional descriptive study was conducted among 300 randomly selected mothers with children <14 years in Awka, Anambra State. A structured questionnaire was used to collect data on sociodemographic factors, self-medication practices, sources of OTC medications, and attitudes toward self-medications. A three–point Likert scale was used to assess the attitude of mothers towards OTC. The data obtained were analysed using the Statistical Package for Social Sciences (SPSS) version 21.0. Sociodemographic variables and self-medication-related variables were summarized using frequency counts, percentages, ranges, means, and standard deviations. Test for association was done using Chi-square test. P-value <0.05 was considered significant at 95% confidence interval. Predictors of self-medication among the study participants were analysed using multivariate logistic regression.
Result: The mean age of the mothers was 33.34 ± 7.54 years, with most under 40 years old. The study found that 82.33% of mothers practiced self-medication, with paracetamol and cough syrups being the most commonly used OTC medications. Sources of information on OTC were mostly from pharmacists and doctors. Significant associations were observed between the practice of self-medication and maternal age (χ2 = 15.556, p = 0.001), number of children (χ2 = 43.178, p = 0.001), and the severity of symptoms (χ2 = 214.915, p = 0.001). Predictors of self-medication included the maternal age 30-39 years, long waiting times, and negative attitudes of healthcare workers (p < 0.05).
Conclusion: The high prevalence of self-medication with OTC drugs among mothers is influenced by various factors, including long waiting times at hospitals, cost considerations, and the attitudes of healthcare workers. To mitigate risks, public health interventions should focus on education, poverty alleviation programs, and stricter regulation of OTC medications. Further studies are recommended to involve a wider population and explore the long-term effects of self-medication in children.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
The Journal is owned, published and copyrighted by the Nigerian Medical Association, River state Branch. The copyright of papers published are vested in the journal and the publisher. In line with our open access policy and the Creative Commons Attribution License policy authors are allowed to share their work with an acknowledgement of the work's authorship and initial publication in this journal.
This is an open access journal which means that all content is freely available without charge to the user or his/her institution. Users are allowed to read, download, copy, distribute, print, search, or link to the full texts of the articles in this journal without asking prior permission from the publisher or the author.
The use of general descriptive names, trade names, trademarks, and so forth in this publication, even if not specifically identified, does not imply that these names are not protected by the relevant laws and regulations. While the advice and information in this journal are believed to be true and accurate on the date of its going to press, neither the authors, the editors, nor the publisher can accept any legal responsibility for any errors or omissions that may be made. The publisher makes no warranty, express or implied, with respect to the material contained herein.
TNHJ also supports open access archiving of articles published in the journal after three months of publication. Authors are permitted and encouraged to post their work online (e.g, in institutional repositories or on their website) within the stated period, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See The Effect of Open Access). All requests for permission for open access archiving outside this period should be sent to the editor via email to editor@tnhjph.com.
How to Cite
References
Hughes CM, McElnay JC, Fleming GF. Benefits and risks of self-medication. Drug safety 2001, 24(14) :1027-37.
Ruiz ME. Risks of self-medication practices. Curr Drug safety, 2010; 5(4): 315-323. Doi:10.2174/157488610792245966.
World Health Organization. The role of the pharmacist in self-care and self-medication: report of the 4th WHO Consultative Group of the role of pharmacist, The Hangue, The Netherlands. WHO; August 1998:26-28.
Federation International de Farmacia. The world self-medication Industry, Joint Statement: Responsible Self Medication. 1999. Available from http://www.wsmi.org/pdf/FIP.pdf.Accessed March, 2022.
Vizhi SK, Senapathi.R. Evaluation of the perception, attitude and practice of self-medication among business students in 3 selected cities, South India. International J of Enterprise and Innovation Management Studies (IJEIMS), 2010; 1(3): 40-4.
Porteous T. Bond C. Hannaford P, Sinclair H. How and why is non-prescription analgesics used in Scotland? Fam Pract, 2005; 22: 78-85.
Lee D, Balasubramaniam K, Ali. H. Drug utilization studies. Their transferability between industrialized and developing countries, WHO Reg Publ. Eur Ser, 1993; 45: 193-3.
Hernandez-Juyol M, Job-Quesada JR. Dentistry and self-medication: A current challenge. Med Oral, 2002; 7:344-7.
Dawood OT, Hassali MA, Saleem F, Ibrahim IR, Addulameer AH, Jasim HH. Assessment of health seeking behavior and self-medication among general public in the state of Penang. Malaysia. Pharm Pract (Granada), 2017;15(3). Doi :10.18549/PharmPract.2017.03.991
Elbur A, Almalki NH, Alghamdi AA. Knowledge, attitudes and practices on medication use and safety among Saudi people: a public-based versus an internet-based survey in Taif; Kingdom of Saudi Arabia. Saudi j Med Pharm Sci, 2016; 2:99-103. Doi: 10.21276/sjmps.2016.2.6.3
Lee HN, Kwak YH, Jung JY. Are parents reliable for diagnosis of serious bacterial infections among children with fever without an apparent source? Medicine 2019; 98(42). Doi:10.1097/MD.0000000000017530.
Araoye, M.O. Sample Size Determination in Research Methodology with Statistics for Health and Social Sciences. Nathadex Publishers, Ilorin, 2004; 115-121
Muoneke VU, Mbachu CO, Bismarck Eke C, Muoneke VU, Una AF, Mbachu C, et al. Caregivers’ Perception and Practice of Self-medication for Fevers in Under-five Children: A Cross-sectional Study in a Rural Community, South-East Nigeria. J Adv Med Med Res 2018; 27:1–12.
Barbi E, Marzuillo P, Neri E, Naviglio S. Fever in children: Pearls and pitfalls. Children 2017;4(9):81. Doi:10.3390/children4090081.
Pileggi C, Mascaro V, Bianco A, Pavia M. Over the counter drugs and complementary medication use among children in South Italy. Biomed Research International 2015: 413912. http://doi.org/10.1155/2015/413912
Albsoul –Younes A, Tahaineh L, Moumani B.Parents’ Knowledge Perception and practices of over the counter medicines used for their children. Jordan J Pharmaceutical Sci 2011;4(3): 181-8.
Tryannovska M, Manias E, Cranswick N, Johnsto. Use of over-the-counter medications for young children in Australia. J Paediatr and Child Health 2010; 46(1-2): 5-9. Doi:10.1111/j.1440-1754.2009. 01609.x
Egbokhare FO, Oyetade SO. Harmonization and standardization of Nigerian Languages. CASAS 2002, pg 106. ISBN 1-919799-70-2.
Anambra State: Subdivisionwww.citypopulation.de. Accessed 24 May,2024.
Barry HR. Clinical and drug poisoning. Nelson WE, Behramanv RE, Kliegman RM, Arvin AM 2010, WD. Sanders Company, Philadelphia, 2013; 18.
Koji EM, Gebretekle GB, Tekle TA. Practice of over-the-counter dispensary of antibiotics for childhood illnesses in Addis Ababa, Ethiopia. A simulated patient encounter study. Antimicrobial Resist Infect Control 2019; 8:119. https://doi.org/10.1186/s13756-019-0571-x
Xu J, Wang X, Sun KS, Lin L, Zhou X. Parental self-medication with antibiotics for children promotes antibiotic over- prescribing in clinical setting in China. Antimicrobial Resist Infect control 2020; 9:150. https://doi.org/10.1186/s13756-020-00811-9