Prevalence of Tuberculosis, Rifampicin resistant Tuberculosis and associated risk factors in Presumptive Tuberculosis patients attending some hospitals in Kaduna, Nigeria
DOI:
https://doi.org/10.60787/tnhj.v23i2.663Keywords:
Tuberculosis, Rifampicin resistance, GeneXpert, Ziehl Neelsen test, Risk factors, Kaduna StateAbstract
Background: This study was carried out to determine the prevalence of Tuberculosis and Mycobacterium tuberculosis resistance to Rifampicin using GeneXpert in presumptive tuberculosis patients attending some hospitals in Kaduna, Nigeria.
Methods: The study design was cross sectional. A total of 198 sputum samples were collected from participants who had been administered questionnaires and screened using Ziehl Neelsen Acid Fast Bacilli (ZN AFB) method and GeneXpert molecular technique. Data obtained from this study was analysed using the Statistical Package for the Social Sciences 23(SPSS® package version 23 Inc. Chicago Illinois, USA).
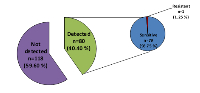
Results: Data obtained showed that using GeneXpert technique, the overall prevalence of TB and Rifampicin resistant TB (RRTB) was 40.4% and 1.25% respectively. A higher prevalence rate was reported among male subjects (47.2%), age group 31-40 (50.9%), those who earned less than 20,000 Naira monthly (41.8%), HIV positive subjects (54.5%), subjects that smoke cigarettes (72.2%) and those that had previous contact with someone living with TB infection (82.4%). The independent variables that were significantly associated with the rate of occurrence of TB (p<0.05 at 95% C.I) were age, gender, HIV status, smoking behaviour, and previous contact with someone having TB.
Conclusions: This study indicates high burden of TB and a low burden of rifampicin resistant tuberculosis among the participants. It highlights the need for rapid detection of TB and Rifampicin resistant strains using GeneXpert or other molecular techniques for TB diagnosis as key to early access to therapy; it will also improve treatment outcomes and decrease transmission rates.
Downloads
References
World Health Organization. Global tuberculosis report 2015 [Internet]. World Health Organization; 2015
World Health Organization. Global Tuberculosis Report 2020 [Internet]. 2020 [cited 2022 Mar 31]. 232 p.
World Health Organization. Global Tuberculosis Report 2017. World Health Organization; 2017. 260 p.
World Health Organization. Global tuberculosis report 2019 [Internet]. 2019 [cited 2022 Mar 31]. 283 p. Available from: https://www.who.int/publications-detail-redirect/9789241565714
Grobbelaar M, Louw GE, Sampson SL, van Helden PD, Donald PR, Warren RM. Evolution of rifampicin treatment for tuberculosis. Infect Genet Evol. 2019 Oct;74:103937.
Beloor Suresh A, Rosani A, Wadhwa R. Rifampin. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 [cited 2022 Mar 30]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK557488/
Longo VD, Shadel GS, Kaeberlein M, Kennedy B. Replicative and Chronological Aging in Saccharomyces cerevisiae. Cell Metabolism. 2012 Jul 3;16(1):18–31.
Pinto L, Menzies D. Treatment of drug-resistant tuberculosis. Infection and drug resistance. 2011;4:129.
Malenfant JH, Brewer TF. Rifampicin Mono-Resistant Tuberculosis-A Review of an Uncommon But Growing Challenge for Global Tuberculosis Control. Open Forum Infect Dis. 2021 Feb;8(2):ofab018.
Fu H, Lewnard JA, Frost I, Laxminarayan R, Arinaminpathy N. Modelling the global burden of drug-resistant tuberculosis avertable by a post-exposure vaccine. Nat Commun. 2021 Jan 18;12(1):424.
Lawson L, Habib AG, Okobi MI, Idiong D, Olajide I, Emenyonu N, et al. Pilot study on multidrug resistant tuberculosis in Nigeria. Ann Afr Med. 2010 Sep;9(3):184–7.
Bello LA, Shittu MO, Shittu BT, Oluremi AS, Akinnuroju ON, Adekola SA. Rifampicin-monoresistant Mycobacterium tuberculosisamong the patients visiting chest clinic, state specialist hospital, Akure, Nigeria. Int J Res Med Sci. 2014;2:1134–7.
Rikoto JA. Pattern of first-line anti-tuberculosis drug resistance and associated factors in patients attending national tuberculosis and leprosy training centre and referral hospital Zaria. 2015 PhD thesis: Zaria. Nigeria: Ahmadu Bello University. 2015;
Audu E, Gambo M, Yakubu A. Rifampicin resistant mycobacterium tuberculosisin Nasarawa State, Nigeria. Niger J Basic Clin Sci. 2017;14(1):21.
Cepheid Gene Xpert Manual. Laboratory Considerations for Use of Cepheid Xpert MTB/RIF Assay. 2013;7.
National Population Comission. State Population, 2006 -Nigeria Data Portal. 2006 [cited 2022 Mar 30]; Available from: https://nigeria.opendataforafrica.org/ifpbxbd/state-population-2006
Lachenbruch PA, Lwanga SK, Lemeshow S. Sample Size Determination in Health Studies: A Practical Manual. Journal of the American Statistical Association. 1991 Dec;86(416):1149.
Stop TB Partnership. guideforprovidingtechnicalsupport_gb.indd. 2013.
Kassa GM, Merid MW, Muluneh AG, Fentie DT. Sputum smear grading and associated factors among bacteriologically confirmed pulmonary drug-resistant tuberculosis patients in Ethiopia. BMC InfectiousDiseases. 2021 Mar 5;21(1):238.
Dinic L, Akande P, Idigbe E, Ani A, Onwujekwe D, Oche A, et al. Genetic Determinants of Drug-Resistant Tuberculosis among HIV-Infected Patients in Nigeria [Internet]. 2012 [cited 2022 Mar 31]. Available from: https://journals.asm.org/doi/epub/10.1128/JCM.00982-12
Butt T, Ahmad RN, Kazmi SY, Rafi N. Multi-drug resistant tuberculosis in Northern Pakistan. JOURNAL-PAKISTAN MEDICAL ASSOCIATION. 2004;54:469–71.
Oyefabi A, Adetiba E, Leeshak E, Adesigbin O. Tuberculosis and the determinants of treatment outcome in Zaria, North Western Nigeria–A nine-year (2007–2015) epidemiological review. Journal of Medicine in the Tropics. 2017;19(2):116.
Denue B, Miyanacha W, Wudiri Z, Alkali M, Goni B, Akawu C. Molecular detection of sputum Mycobacterium tuberculosis/rifampicin resistance among presumptive pulmonary tuberculosis cases in Borno state, North-Eastern Nigeria. Port Harcourt Med J. 2018;12(2):64.
Vange O, Umeh EU, Azua ET. The prevalence of tuberculosis and rifampicin resistance among the Mycobacterium tuberculosisclinical isolates at Federal Medical Centre Makurdi, Benue State, Nigeria. African Journal of Microbiology Research. 2019;13(11):214–8.
Babajide TI, Nwadike VU, Ojo DA, Onasanya OA, Ojide KC, Kula IE. Prevalence of Tuberculosis among patients attending two Secondary Hospitals in Abeokuta Ogun State. African Journal of Clinical and Experimental Microbiology. 2014;15(3):144–50.
Kooffreh ME, Offor JB, Ekerette EE, Udom UI. Prevalence of tuberculosis in Calabar, Nigeria: A case study of patients attending the outpatients Department of Dr. Lawrence Henshaw Memorial Hospital, Calabar. Prevalence. 2016;5(3):130–3.
Mulu W, Abera B, Yimer M, Hailu T, Ayele H, Abate D. Bacterial agents and antibiotic resistance profiles of infections from different sites that occurred among patients at Debre Markos Referral Hospital, Ethiopia: a cross-sectional study. BMC Research Notes. 2017 Jul 6;10(1):254.
Rasaki SO, AJibola AIA, Musa SA, Moradeyo AK, Odeigah LO, Abdullateef SG, et al. Rifampicin resistant tuberculosis in a secondary health institution in Nigeria, West Africa. Journal of Infectious Diseases and Therapy. 2014;
Okonko IO, Soleye FA, Adeniji FO, Okerentugba PO. HIV and TB co-infection among patients on directly observed treatment of short course in Abeokuta, Ogun State, Nigeria. Age. 2012;20(09):20.
Schurz H, Salie M, Tromp G, Hoal EG, Kinnear CJ, Möller M. The X chromosome and sex-specific effects in infectious disease susceptibility. Human genomics. 2019;13(1):1–12.
Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016 Oct;16(10):626–38.
Klein SL, Marriott I, Fish EN. Sex-based differences in immune function and responses to vaccination. Trans R Soc Trop Med Hyg. 2015 Jan;109(1):9–15.
Nwachokor FN, Thomas JO. Tuberculosis in Ibadan, Nigeria--a 30 year review. Cent Afr J Med. 2000 Nov;46(11):287–92.
Alau KK, Weaver MR, Ogungbemi MK, Ashefor G, Anenih J, Adeyemi A. Prevalence of tuberculosis and HIV/AIDS co-infection among HIV clients at global fund supported comprehensive facilities in Nigeria. International Journal of Research in Medical Science. 2016;4(6):91–5.
Okodua M, Ihongbe J, Esumeh F. Pulmonary tuberculosis and resistance pattern to first line anti-tuberculosis drugs in a city of western Nigeria. International Journal of Basic, Applied and Innovative Research. 2012;1(2):48–56.
Al-Hajoj S, Varghese B, Shoukri MM, Al-Omari R, Al-Herbwai M, AlRabiah F, et al. Epidemiology of Antituberculosis Drug Resistance in Saudi Arabia: Findings of the First National Survey. Antimicrob Agents Chemother. 2013 May;57(5):2161–6.
Agrawal M, Bajaj A, Bhatia V, Dutt S. Comparative Study of GeneXpert with ZN Stain and Culture in Samples of Suspected Pulmonary Tuberculosis. J Clin Diagn Res. 2016 May;10(5):DC09-12.
Federal Ministry of Health. Federal Ministry of Health (2015). Department of Public Health. National Tuberculosis and Leprosy Control Programme. AFB Microscopy Training Manual. Page 8-70.
Ogbo FA, Ogeleka P, Okoro A, Olusanya BO, Olusanya J, Ifegwu IK, et al. Tuberculosis disease burden and attributable risk factors in Nigeria, 1990–2016. Tropical Medicine and Health. 2018 Sep 25;46(1):34.
Jee SH, Golub JE, JoJ, Park IS, Ohrr H, Samet JM. Smoking and risk of tuberculosis incidence, mortality, and recurrence in South Korean men and women. Am J Epidemiol. 2009 Dec 15;170(12):1478–85.
Bronner Murrison L, Martinson N, Moloney RM, Msandiwa R, Mashabela M, Samet JM, et al. Tobacco Smoking and Tuberculosis among Men Living with HIV in Johannesburg, South Africa: A Case-Control Study. PLoS One. 2016 Nov 28;11(11):e0167133.
O’Leary SM, Coleman MM, Chew WM, Morrow C, McLaughlin AM, Gleeson LE, et al. Cigarette smoking impairs human pulmonary immunity to Mycobacterium tuberculosis. Am J Respir Crit Care Med. 2014 Dec 15;190(12):1430–6.
World Health Organization. Global tuberculosis report 2016 [Internet]. World Health Organization; 2016 [cited 2022 Mar 30]. 142 p. Available from: https://apps.who.int/iris/handle/10665/250441
Jurcev-Savicevic A, Mulic R, Kozul K, Ban B, Valic J, Bacun-Ivcek L, et al. Health system delay in pulmonary tuberculosis treatment in a country with an intermediate burden of tuberculosis: a cross-sectional study. BMC Public Health. 2013 Mar 21;13(1):250.
Adesokan H, Cadmus E, Adeyemi W, Lawal O, Ogunlade CO, Osman E, et al. Prevalence of previously undetected tuberculosis and underlying risk factors for transmission in a prison setting in Ibadan, south-western Nigeria. Afr J Med Med Sci. 2014 Sep;43(Suppl 1):45–50.
Lönnroth K, Williams BG, Stadlin S, Jaramillo E, Dye C. Alcohol use as a risk factor for tuberculosis –a systematic review. BMC Public Health. 2008 Aug 14;8(1):289.
Idigbe O, Sofola T, Akinosho R, Onwujekwe D, Odiah F, Okoye R. Initial drug resistance tuberculosis amongst HIV seropositive and seronegative prison inmates in Lagos, Nigeria. In: Int Conf AIDS. 1998. p. 137.
Fadeyi A, Desalu OO, Ugwuoke C, Opanwa OA, Nwabuisi C, Salami AK. Prevalence of Rifampicin-Resistant Tuberculosis among Patients Previously Treated for Pulmonary Tuberculosis in North-Western, Nigeria. Niger Med J. 2017 Dec;58(6):161–6.
Ukwamedua H, Omote V, Etaghene J, Oseji ME, Agwai IC, Agbroko H. Rifampicin resistance among notified pulmonary tuberculosis (PTB) cases in South-Southern Nigeria. Heliyon. 2019;5(7):e02096.
Menon S, Dharmshale S, Chande C, Gohil A, Lilani S, MohammadS, et al. Drug resistance profiles of Mycobacterium tuberculosisisolates to first line anti-tuberculous drugs: A five years study. Lung India. 2012;29(3):227–31.
Ikuabe PO, Ebuenyi ID. Prevalence of rifampicin resistance by automated Genexpert rifampicin assay in patients with pulmonary tuberculosis in Yenagoa, Nigeria. Pan Afr Med J. 2018 Apr 6;29:204.
Caminero JA. Multidrug-resistant tuberculosis: epidemiology, risk factors and case finding. Int J Tuberc Lung Dis. 2010 Apr;14(4):382–90.
Downloads
Published
Versions
- 2023-08-25 (2)
- 2023-07-10 (1)
How to Cite
Issue
Section
License
Copyright (c) 2023 Journal and Publisher

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Journal is owned, published and copyrighted by the Nigerian Medical Association, River state Branch. The copyright of papers published are vested in the journal and the publisher. In line with our open access policy and the Creative Commons Attribution License policy authors are allowed to share their work with an acknowledgement of the work's authorship and initial publication in this journal.
This is an open access journal which means that all content is freely available without charge to the user or his/her institution. Users are allowed to read, download, copy, distribute, print, search, or link to the full texts of the articles in this journal without asking prior permission from the publisher or the author.
The use of general descriptive names, trade names, trademarks, and so forth in this publication, even if not specifically identified, does not imply that these names are not protected by the relevant laws and regulations. While the advice and information in this journal are believed to be true and accurate on the date of its going to press, neither the authors, the editors, nor the publisher can accept any legal responsibility for any errors or omissions that may be made. The publisher makes no warranty, express or implied, with respect to the material contained herein.
TNHJ also supports open access archiving of articles published in the journal after three months of publication. Authors are permitted and encouraged to post their work online (e.g, in institutional repositories or on their website) within the stated period, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See The Effect of Open Access). All requests for permission for open access archiving outside this period should be sent to the editor via email to editor@tnhjph.com.








